Sleep Deprivation Taxes Neurons, Racks Up Brain Aβ?
Quick Links
While the occasional all-nighter to cram for exams or finish a grant proposal may seem like no big deal, losing sleep night after night could take its toll on brain health in later life, two new studies suggest. Based on microdialysis experiments in live mice, Dave Holtzman, Washington University, St. Louis, Missouri, and colleagues report that extracellular amyloid-β levels in the brain fall during slumber and rise with wakefulness. They discovered that these Aβ dynamics rely on the hormone orexin, and that forcing animals to sleep or stay awake decreases or increases Aβ plaque formation accordingly in a mouse model for Alzheimer disease. Holtzman presented some of these findings last year at the Human Amyloid Imaging meeting in Chicago (see ARF conference story). The full report was published online yesterday in Science.
Earlier work from the Holtzman lab had shown that synaptic activity triggers Aβ release (Cirrito et al., 2005 and ARF related news story), suggesting that the sleep-deprived mice in the current study churned out more Aβ because their brains were revved up longer than usual. While this is hard to prove formally, a rat electrophysiology study published in yesterday’s issue of Neuron seems to lend support for that idea. Led by Giulio Tononi at the University of Wisconsin-Madison, researchers report that neuronal firing in the brain is lower during sleep, and that the firing drops or escalates further the longer an animal has been asleep or awake. “This may tie in very much to why we see Aβ levels higher during wake and lower during sleep, and help explain why sleep deprivation is harmful not only for neuronal function but also may lead to an increase in Aβ levels and amyloid accumulation over time,” Holtzman noted in an e-mail to ARF.
Holtzman and colleagues did not start thinking about sleep from the get-go. They were trying to get a handle on Aβ pathogenesis by studying how the peptide gets metabolized in the brain. Lead author Jae-Eun Kang and coworkers had shown that stress drives up extracellular Aβ levels (Kang et al., 2007 and ARF related news story), but wondered what happens under normal conditions. Using microdialysis techniques to measure brain interstitial fluid (ISF) Aβ in Tg2576 mice, the researchers were at first puzzled to see peptide levels going up or down at various times. Upon closer observation, they discovered a pattern: over a 24-hour period, mean Aβ levels were about 25 percent lower during the day than at night. With help from sleep experts at Stanford University, Palo Alto, California, the team rigged mice with electroencephalogram (EEG) electrodes to record waking and sleeping. They found that “it wasn’t light and dark but rather how long the animals had been awake that seemed to correlate best with levels of Aβ peptide,” Holtzman told ARF. The longer the animal had been awake, the higher the ISF Aβ levels, and vice versa for amount of time spent sleeping. This pattern held in wild-type mice and in young male volunteers whose cerebrospinal fluid Aβ levels were measured by lumbar catheters (see also Bateman et al., 2007). As such, the daily Aβ changes appeared to reflect normal physiology.
The researchers then determined the effect on ISF Aβ of forcing mice to stay up past their bedtime—a regimen perhaps equally grueling to the researcher who had to stand by for six hours using a paintbrush to rouse animals on the verge of dozing. “This was no trivial study. It took three years,” Holtzman said. The tedious monitoring paid off, however, with data showing higher ISF Aβ levels during sleep deprivation (compared to peptide levels 24 hours prior) and an immediate drop in Aβ once the animals were finally allowed to sleep.
Reasoning that higher levels of ISF Aβ tend to make the peptide more likely to aggregate over time, the researchers subjected AD transgenic mice (APPswe/PS1dE9) to chronic sleep deprivation to see the effect on brain Aβ deposition. They used mice that had not yet developed amyloid pathology, and kept them awake 20 hours daily for 21 days by placing them on a special platform that sends snoozers into a pool of water. As predicted, sleep-restricted animals had greater plaque deposition in multiple cortical regions, compared to animals that slept at will. Extrapolating to humans, the data “suggest that midlife sleep abnormalities may predispose you to a neurodegenerative disease,” Holtzman told ARF.
Furthermore, the researchers determined that the daily Aβ fluctuations are regulated by orexin, a hormone that stimulates wakefulness. When the researchers gave mice six-hour brain infusions of orexin at a time they would normally be asleep, ISF Aβ was elevated relative to peptide levels measured during the same period 24 hours prior. Conversely, mice treated with a compound that blocks orexin signaling slept more and had lower Aβ levels. These findings suggest the orexin pathway as a potential target for AD prevention, Holtzman said. Sleep disturbances are common in several neurodegenerative diseases (see Gagnon et al., 2008, for review), and research suggests that improving sleep and circadian rhythm in dementia patients may also improve their cognition (Ancoli-Israel et al., 2008; Riemersma-van der Lek et al., 2008 and ARF related news story).
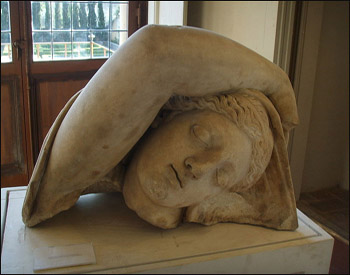
Greek mythology offers different versions of what happened during the famous sleeping episode of King Minos's daughter, the goddess Ariadne, on the island of Naxos, which artists immortalized on vases, paintings, and this Roman sculpture. Most versions have to do with rivalry between Theseus and Dionysus. But forget the guys. Maybe Ariadne was simply giving her synapses a well-deserved rest from the tiring love triangle, the better to keep her brain Aβ levels down? Image credit: Creative Commons
Those findings seem to jibe with recent work by University of Wisconsin-Madison researchers, including Tononi, who propose that sleep is needed to refresh synapses overworked from the day’s activity (Gilestro et al., 2009 and ARF related news story). In that study, the scientists tracked synaptic markers in flies, finding that these proteins rise with sleep deprivation and fall during slumber. One drawback with flies, though, is that “you cannot measure the EEG. You cannot record brain waves. And although you can record neurons, it’s much more difficult,” Vladyslav Vyazovskiy, University of Wisconsin-Madison, told ARF. “Studying mammals gives the opportunity to get many more physiological measures.”
For the Neuron paper, first author Vyazovskiy and colleagues used rats, implanting their brains with electrodes thin enough to record just a few neurons at a time. They measured several parameters of neuronal firing, including frequency, synchrony, and the relationship between firing patterns and various sleep phases. Whereas other studies had compared neuronal activity in sleep and wake states, the researchers suspected that activity levels may differ not only depending on sleep-wake state but also on how long the animal had been awake or asleep. For example, “in the morning, you wake up and you are fresh and well-rested,” Vyazovskiy said. “In the evening, you are also awake, but you are tired and sleepy.”
Vyazovskiy and colleagues found that neurons fired at progressively higher frequencies the longer the rats stayed awake, and that firing rates dropped correspondingly the longer the animals were asleep. Given that neuronal activity is “very costly in terms of energy,” Vyzovskiy said, one tenet of the so-called synaptic homeostasis hypothesis is that sleep serves to downscale synapses—to control the metabolic costs of neuronal function. “We provide new support for this hypothesis by looking at the behavior of single neurons,” he told ARF.—Esther Landhuis
References
News Citations
- HAI Chicago: PIB and Aβ Show Regional Nuances and Sleep-Wake Rhythm
- Paper Alert: Synaptic Activity Increases Aβ Release
- Stress and Aβ—A Fluid Connection in Mice
- Research Brief: Beefing Up Circadian Rhythm Helps AD Symptoms
- Sleep Settles Strained Synapses, Keeps Aβ Levels at Bay?
Paper Citations
- Cirrito JR, Yamada KA, Finn MB, Sloviter RS, Bales KR, May PC, Schoepp DD, Paul SM, Mennerick S, Holtzman DM. Synaptic activity regulates interstitial fluid amyloid-beta levels in vivo. Neuron. 2005 Dec 22;48(6):913-22. PubMed.
- Kang JE, Cirrito JR, Dong H, Csernansky JG, Holtzman DM. Acute stress increases interstitial fluid amyloid-beta via corticotropin-releasing factor and neuronal activity. Proc Natl Acad Sci U S A. 2007 Jun 19;104(25):10673-8. PubMed.
- Bateman RJ, Wen G, Morris JC, Holtzman DM. Fluctuations of CSF amyloid-beta levels: implications for a diagnostic and therapeutic biomarker. Neurology. 2007 Feb 27;68(9):666-9. PubMed.
- Gagnon JF, Petit D, Latreille V, Montplaisir J. Neurobiology of sleep disturbances in neurodegenerative disorders. Curr Pharm Des. 2008;14(32):3430-45. PubMed.
- Ancoli-Israel S, Palmer BW, Cooke JR, Corey-Bloom J, Fiorentino L, Natarajan L, Liu L, Ayalon L, He F, Loredo JS. Cognitive effects of treating obstructive sleep apnea in Alzheimer's disease: a randomized controlled study. J Am Geriatr Soc. 2008 Nov;56(11):2076-81. PubMed.
- Riemersma-van der Lek RF, Swaab DF, Twisk J, Hol EM, Hoogendijk WJ, Van Someren EJ. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA. 2008 Jun 11;299(22):2642-55. PubMed.
- Gilestro GF, Tononi G, Cirelli C. Widespread changes in synaptic markers as a function of sleep and wakefulness in Drosophila. Science. 2009 Apr 3;324(5923):109-12. PubMed.
Other Citations
Further Reading
Papers
- Cirrito JR, Kang JE, Lee J, Stewart FR, Verges DK, Silverio LM, Bu G, Mennerick S, Holtzman DM. Endocytosis is required for synaptic activity-dependent release of amyloid-beta in vivo. Neuron. 2008 Apr 10;58(1):42-51. PubMed.
- Cirrito JR, Yamada KA, Finn MB, Sloviter RS, Bales KR, May PC, Schoepp DD, Paul SM, Mennerick S, Holtzman DM. Synaptic activity regulates interstitial fluid amyloid-beta levels in vivo. Neuron. 2005 Dec 22;48(6):913-22. PubMed.
- Kang JE, Cirrito JR, Dong H, Csernansky JG, Holtzman DM. Acute stress increases interstitial fluid amyloid-beta via corticotropin-releasing factor and neuronal activity. Proc Natl Acad Sci U S A. 2007 Jun 19;104(25):10673-8. PubMed.
- Gagnon JF, Petit D, Latreille V, Montplaisir J. Neurobiology of sleep disturbances in neurodegenerative disorders. Curr Pharm Des. 2008;14(32):3430-45. PubMed.
News
- Paper Alert: Synaptic Activity Increases Aβ Release
- Stress and Aβ—A Fluid Connection in Mice
- HAI Chicago: PIB and Aβ Show Regional Nuances and Sleep-Wake Rhythm
- Link Between Synaptic Activity, Aβ Processing Revealed
- Sleep Settles Strained Synapses, Keeps Aβ Levels at Bay?
- Research Brief: Beefing Up Circadian Rhythm Helps AD Symptoms
Primary Papers
- Kang JE, Lim MM, Bateman RJ, Lee JJ, Smyth LP, Cirrito JR, Fujiki N, Nishino S, Holtzman DM. Amyloid-beta dynamics are regulated by orexin and the sleep-wake cycle. Science. 2009 Nov 13;326(5955):1005-7. PubMed.
- Vyazovskiy VV, Olcese U, Lazimy YM, Faraguna U, Esser SK, Williams JC, Cirelli C, Tononi G. Cortical firing and sleep homeostasis. Neuron. 2009 Sep 24;63(6):865-78. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
University of Kentucky
The recent report by Kang et al. suggests not only that amyloid may serve an important role in sleep regulation, but also further highlights the need for additional studies on its physiological role. The study shows that amyloid is at least a biomarker of sleep, but it is interesting to note that it may also provide a mechanistic link mediating orexinergic signaling that pushes brain systems toward sleep. These findings are especially compelling considering other identified physiological effects of amyloid/APP, for example, Aβ feedback synaptic inhibition (Hsieh et al., 2006) or amyloid-enhanced potassium channel conductance (Furukawa et al., 1996). These physiological effects may be linked to slow wave sleep oscillations and neuronal quiescence (Vyazovskiy et al., 2009).
However, it is also important to note that there are likely to be multiple players in sleep regulation. For example, earlier work indicates BDNF and Homer1a also play roles (Faraguna et al., 2008; Mackiewicz et al., 2008), and it will be interesting to see what specific role amyloid may play in the molecular networks associated with sleep. Future studies combining multiple techniques (for instance, EEG, cognition, and microarray) may be particularly well suited for elucidating interactions among complex networks regulating sleep and the consequences of its disruption.
References:
Hsieh H, Boehm J, Sato C, Iwatsubo T, Tomita T, Sisodia S, Malinow R. AMPAR removal underlies Abeta-induced synaptic depression and dendritic spine loss. Neuron. 2006 Dec 7;52(5):831-43. PubMed.
Furukawa K, Barger SW, Blalock EM, Mattson MP. Activation of K+ channels and suppression of neuronal activity by secreted beta-amyloid-precursor protein. Nature. 1996 Jan 4;379(6560):74-8. PubMed.
Vyazovskiy VV, Olcese U, Lazimy YM, Faraguna U, Esser SK, Williams JC, Cirelli C, Tononi G. Cortical firing and sleep homeostasis. Neuron. 2009 Sep 24;63(6):865-78. PubMed.
Faraguna U, Vyazovskiy VV, Nelson AB, Tononi G, Cirelli C. A causal role for brain-derived neurotrophic factor in the homeostatic regulation of sleep. J Neurosci. 2008 Apr 9;28(15):4088-95. PubMed.
Mackiewicz M, Paigen B, Naidoo N, Pack AI. Analysis of the QTL for sleep homeostasis in mice: Homer1a is a likely candidate. Physiol Genomics. 2008 Mar 14;33(1):91-9. PubMed.
University of Toronto
In this work from Dave Holtzman’s lab, the influence of the sleep-wake cycle on Aβ metabolism was explored. The investigators found that brain interstitial fluid levels of Aβ in transgenic mice fluctuated over a 24-hour period with lower levels during sleep and higher levels during wakefulness. Moreover, sleep-depriving the mice caused an increase in plaque load, but this effect could be abolished by treating the mice with Almorexant, a receptor antagonist of orexin—a molecule regulating the sleep-wake cycle. Finally, the researchers also looked at human CSF Aβ levels and found similar alterations over the day. This study provides important new evidence that Aβ formation and plaque deposition can be controlled by affecting the sleep pattern. Also, the work adds a new perspective to the use of CSF Aβ as a diagnostic marker, as the reference values may have to be adjusted to the sampling timepoints.
View all comments by Martin IngelssonMake a Comment
To make a comment you must login or register.