Tau Deepens Cognitive Trouble in Lewy Body Diseases
Quick Links
Clumps of α-synuclein in neurons define Lewy body diseases, but tau tangles may add their own stamp to these disorders. Results from an imaging study, published September 19 in JAMA Neurology, suggest that tau pathology packs a cognitive wallop in people with dementia with Lewy bodies as well as those with Parkinson’s disease dementia. The researchers, led by Stephen Gomperts of Massachusetts General Hospital in Charlestown, also reported that in a few cases, tau pathology occurred in the absence of pathological accumulation of Aβ. The findings, some of which were presented at the International Dementia with Lewy Bodies Conference last year, support the idea that aggregated tau plays a role in the cognitive impairment that occurs in Lewy body diseases.
“This finding underscores the importance of tau accumulation in these disorders,” said Kejal Kantarci of the Mayo Clinic in Rochester, Minnesota. She added that the small size of the study makes replication crucial. Tanis Ferman of the Mayo Clinic in Jacksonville, Florida, agreed. “But this is an important first step to establishing the usefulness of tau imaging biomarkers in patients with Lewy body disease,” she added.
Lewy body diseases (LBDs) include Parkinson’s disease (PD), Parkinson’s disease with dementia (PDD), and dementia with Lewy bodies (DLB). They differ from each other by the order in which cognitive and parkinsonian (motor) symptoms arise (for a review, see Gomperts et al., 2016). While many people with PD only develop motor problems, those with PDD subsequently develop cognitive problems as well. In people with DLB, the symptom onset is reversed: cognitive troubles arise prior to parkinsonism.
Postmortem neuropathological studies have been telling researchers for some time that LBDs are anything but simple, since they do not fall into neat neuropathological categories. In addition to the flagship α-synuclein pathology, many people with LBDs also harbor AD-like neurofibrillary tangles and amyloid plaques. Because postmortem analyses offer but a snapshot of these complex co-pathologies after the fact, researchers now seek to use amyloid and tau imaging to track their interactions as disease progresses.
Last year at IDLBC, Gomperts presented preliminary findings from a small cross-sectional study in a cohort of people with LBDs. It measured Aβ accumulation via PiB retention, tau aggregation via AV-1451 uptake, and performance on the Cognitive Dementia Rating scale sum-of-boxes (CDR-SOB) and the Mini Mental State Examination (MMSE). Seven people had been diagnosed with DLB, eight with PDD, nine with PD, and 29 were cognitively normal controls (see Dec 2015 conference coverage). The main findings—based on single scans of Aβ and tau about two months apart—correlated high levels of tau tracer uptake in the inferior temporal gyrus (ITG) with waning cognition in people with DLB and PDD. Incidentally, the ITG is also the area where tau pathology starts to spread beyond the hippocampal formation in early AD. People with DLB had the most tau. AV-1451 uptake in some DLB patients rivaled that seen in people with AD.
The paper now elaborates on those preliminary findings. The researchers report that higher tau deposition in the ITG, and in the precuneus, correlated with cognitive impairment among the people with PDD and DLB. No such correlation emerged among healthy controls or PD patients. While the amount of tau detected—particularly in those with DLB—varied drastically among patients, its anatomic distribution in the brain was consistent, matching that in people with AD. This similarity suggests that the pathological processes driving tau accumulation in LBD may be similar to those that drive tau accumulation in AD, Gomperts told Alzforum.
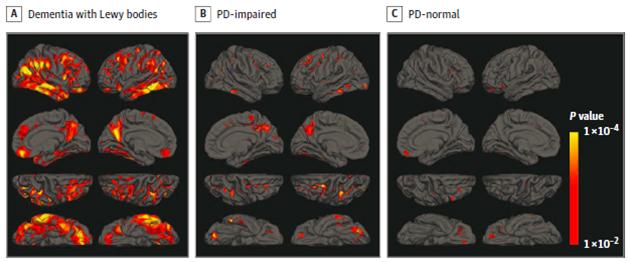
Tracing Tau. People with DLB (left) accumulate more tau than PD patients who are cognitively impaired (middle) or have normal cognition (right). [Courtesy of Gomperts et al., JAMA Neurology 2016.]
However, in people with AD, the spread of tau into the cortex—a move that heralds cognitive impairment—reportedly occurs only after Aβ has accumulated (see Aug 2016 news and Mar 2016 news). Is this true in people with LBDs as well? Not entirely. Of 21 people with LBD, 17 (81 percent) had low amyloid burden. Despite having minimal Aβ, four of these people also had high tau tracer uptake in the ITG. This uncoupling of Aβ and tau, while only occurring in a small group of people, suggests that in LBDs, cortical tauopathy is possible without the extensive Aβ deposition characteristic of AD, Gomperts told Alzforum. He speculated that perhaps a synergistic relationship between α-synuclein and tau incited tauopathy in these patients, who were all cognitively impaired. Such a toxic relationship between the two proteins has been reported in animal models (see Jul 2013 news).
Johannes Attems of Newcastle University in England agreed with that assessment. He pointed out that the existence of moderate tau deposition in the absence of Aβ has been documented before, in people with primary age-related tauopathy (PART). However, PART happens without cognitive impairment, and Aβ is ultimately necessary to drive high levels of tau as well as cognitive impairment (i.e., AD). “Therefore, the most likely neuropathological correlate for dementia in the group with low amyloid burden and higher than normal tau burden in the inferior temporal gyrus in this study is α-synuclein pathology,” he commented.
Interestingly, the researchers also reported that in the DLB group, greater tau deposition in the ITG and precuneus associated with a shorter disease duration. This suggests that tau aggregation accelerates the progression of disease, said Gomperts. No correlation emerged between Aβ deposits and cognition across all groups.
The findings dovetailed with Ferman’s previous postmortem neuropathological analyses: DLB had progressed fastest in people with most tauopathy at autopsy. “[Gomperts’] study provides evidence that tau deposition can be measured in living patients with DLB and PD dementia, and that those with greater tau deposition tend to have greater cognitive impairment and greater dementia severity,” Ferman concluded.
To take full advantage of the benefits of live tau imaging, Gomperts plans to track the spread of tau pathology in people with LBDs over time.—Jessica Shugart
References
News Citations
- Dementia with Lewy Bodies: Sharper Image for a Formerly Blurry Disease
- Brain Imaging Suggests Aβ Unleashes the Deadly Side of Tau
- Tau PET Aligns Spread of Pathology with Alzheimer’s Staging
- An Extra Strain on the Brain—α-Synuclein Seeds Tau Aggregation
Paper Citations
- Gomperts SN. Lewy Body Dementias: Dementia With Lewy Bodies and Parkinson Disease Dementia. Continuum (Minneap Minn). 2016 Apr;22(2 Dementia):435-63. PubMed.
Further Reading
Papers
- Marquié M, Normandin MD, Vanderburg CR, Costantino IM, Bien EA, Rycyna LG, Klunk WE, Mathis CA, Ikonomovic MD, Debnath ML, Vasdev N, Dickerson BC, Gomperts SN, Growdon JH, Johnson KA, Frosch MP, Hyman BT, Gómez-Isla T. Validating novel tau positron emission tomography tracer [F-18]-AV-1451 (T807) on postmortem brain tissue. Ann Neurol. 2015 Nov;78(5):787-800. Epub 2015 Sep 25 PubMed.
- Gomperts SN, Marquie M, Locascio JJ, Bayer S, Johnson KA, Growdon JH. PET Radioligands Reveal the Basis of Dementia in Parkinson's Disease and Dementia with Lewy Bodies. Neurodegener Dis. 2016;16(1-2):118-24. Epub 2015 Dec 8 PubMed.
Primary Papers
- Gomperts SN, Locascio JJ, Makaretz SJ, Schultz A, Caso C, Vasdev N, Sperling R, Growdon JH, Dickerson BC, Johnson K. Tau Positron Emission Tomographic Imaging in the Lewy Body Diseases. JAMA Neurol. 2016 Nov 1;73(11):1334-1341. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
Mayo Clinic
The primary pathologic feature of DLB and PD dementia involves the accumulation of α-synuclein, but a subset of patients also have varying degrees of amyloid and tau deposition. It is important to be able to detect and track these pathologies during life in order to understand how they contribute to the clinical features of the disease, but also to be able to monitor the effectiveness of emerging treatments that target these specific pathologies. This study by Gomperts et al. provides evidence that tau deposition can be measured in living patients with DLB and PD dementia, and that those with greater tau deposition tend to have greater cognitive impairment and greater dementia severity. Even though the overall tau aggregation is lower than what is typically seen in Alzheimer’s disease, this relationship suggests that tau deposition contributes meaningfully to the dementia associated with Lewy body disease. Replication is certainly needed, but this is an important first step to establishing the usefulness of this tau imaging biomarker in patients with Lewy body disease.
Mayo Clinic
The paper by Gomperts et al. is an important investigation of AV-1451 binding in Lewy body dementias. Accumulation of tau pathology in patients with DLB has been recognized through autopsy studies. The study demonstrates that tau deposition is present in patients with Lewy body disease who have cognitive impairment. This is particularly true in cases of dementia with Lewy bodies (DLB) and underscores the importance of tau accumulation in Lewy body diseases.
The limited sample size (n <10) in each clinical group calls for confirmation of findings in a larger sample. Furthermore, the absence of a relationship between amyloid deposition and tau deposition in DLB is unexpected and may be impacted by the small number of cases in the study. Understanding the accumulation of amyloid and tau in Lewy body diseases is critical for multitarget treatment strategies in these disorders.
Newcastle University
The findings of this in vivo imaging study are consistent with data from neuropathologic postmortem studies and once again highlight the fact that the aging human brain is frequently characterized by the presence of multiple pathologies. It is very important for all researchers in the field to be aware of this cerebral multimorbidity as it implies that seemingly homogenous patient cohorts (e.g., AD) may in fact show heterogenous neuropathologies (e.g., AD with and without concomitant TDP-43 pathology).
The authors found considerable cortical tau pathology in the absence of elevated Aβ in the DLB group, suggesting a synergistic interaction between α-synuclein and tau pathology, which has been suggested by transgenic animal studies and human postmortem studies. However, the absence of a statistically significant correlation between cortical amyloid and tau burden does not per se preclude an influence of Aβ on tau in these cases, as it has been demonstrated that specific amyloid subspecies (e.g., pyroglutamylated Aβ, phospho Aβ), rather that general Aβ burden, have an aggravating effect of tau pathology.
Four out of 17 Lewy body disease cases with low amyloid burden showed higher tau burden than normal controls in the inferior temporal gyrus; this finding is consistent with neuropathological data clearly demonstrating that Aβ is not necessary for the development of tau pathology. Indeed, a diagnostic category termed primary age-related tauopathy (PART) has recently been described. PART is characterized by the presence of tau pathology up to Braak stage IV and either complete lack of (definite PART) or very low (possible PART) Aβ pathology, respectively. Of note, PART cases (without other pathology) are usually not cognitively impaired and high Braak stages V/VI (which are cognitively impaired) have not been observed without Aβ, suggesting that Aβ is necessary for the development of end-stage high-tau pathology. Therefore, the most likely neuropathological correlate for dementia in the group with low amyloid burden and higher than normal tau burden in the inferior temporal gyrus in this study is α-synuclein pathology.
In conclusion, this is an exciting study that should stimulate future research in which the age-associated neurodegenerative condition is not simply categorized according to disease groups, but rather described according to the neuropathological changes present in the individual human brain. While such an approach is already pursued in neuropathological postmortem studies, further diagnostic tools are needed to follow this path in clinical in vivo studies.
Make a Comment
To make a comment you must login or register.