Gotta Get Rid of It All: Total Plaque Clearance Key for Clinical Benefit
Quick Links
As researchers parse what makes amyloid immunotherapy work, one answer keeps bubbling up: Take out all plaque quickly, so that clinical benefits have time to show up. At last month’s Clinical Trials on Alzheimer’s Disease conference, held October 24 to 27 in Boston and online, several talks added heft to this emerging view. Scientists at Eli Lilly correlated amyloid negativity early on in their Phase 3 donanemab trial with slowed tangle buildup by its end. This partially answered the nagging question of how the study could have achieved a therapeutic effect without budging tangles overall. Data from other programs reinforced that what matters is not just how much plaque is removed, but how low it gets, and how soon.
- In donanemab Phase 3, those whose plaque was gone by one year accumulated fewer tangles.
- Across immunotherapy trials, seeing clinical benefits hinges on clearing plaque a year before the trial ends.
- Lecanemab injected under the skin removes more plaque than do infusions.
“Amyloid removal to the normal range is the best predictor of efficacy, and is directly proportional to the magnitude of the effect,” Randall Bateman of Washington University in St. Louis said in Boston. Noting that tau PET findings have been less consistent so far, he added, “We still have an enormous amount to learn.”
Meanwhile, a meta-analysis found that amyloid immunotherapies work equally well in APOE4 carriers and noncarriers, while Eisai scientists said a subcutaneous formulation gets more lecanemab into the blood than does the intravenous version, though at the price of correspondingly higher ARIA. These data reflect the field's current effort to hone anti-amyloid therapy toward use in clinics around the country.
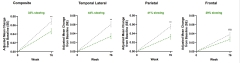
Tangles Lag Amyloid Removal. In the donanemab Phase 3 trial, people free of plaque within one year (green) had fewer tangles throughout the brain six months later than matched placebo controls (gray). [Courtesy of Eli Lilly.]
All Signs Point to Plaque Clearance
Tangle accumulation has slowed in all successful anti-amyloid antibody trials so far—except in the Trailblazer-Alz2 study of donanemab. That trial posted the highest efficacy reported to date for amyloid immunotherapy, holding back decline on the CDR-SB by 36 percent, yet without an apparent effect on tangles (Jul 2023 conference news). Many scientists were nonplussed by this (Aug 2023 conference news).
In Boston, Lilly’s Sergey Shcherbinin offered post hoc evidence that donanemab does curb tangles if you wait long enough after plaques are gone. Shcherbinin analyzed data from Trailblazer-Alz2’s “combined tau” cohort, i.e., all participants in the trial’s placebo-controlled portion. Initially comprising 1,736 people, this group had baseline tau PET scans above 1.10 SUVR and, after one year on donanemab, two-thirds were below the amyloid positivity threshold of 24.1 centiloids. Shcherbinin wanted to compare the magnitude of their treatment effect at 18 months with that of the whole cohort.
The researchers had a problem, however. They could not simply compare the “rapid clearance” group to the placebo group, because people whose plaque vanishes quickly may have different baseline characteristics than those whose plaque is harder to budge. Indeed, compared with the trial’s overall cohort, “rapid clearers” were a year older, slightly less likely to carry APOE4, and started with less plaque, 95 centiloids rather than 103. Their baseline tau PET averaged 1.31 SUVR, versus 1.34 in the cohort overall. To account for these differences, researchers matched up the 390 rapid clearers with 390 placebo controls of similar age, APOE genotype, and amyloid and tau load at baseline.
How did rapid clearers measure up? On cognitive tests, they eked out about the same small benefit as did the Trailblazer-Alz2 cohort as a whole, declining 34 percent less on the iADRS and CDR-SB than did their matched controls. On tau PET, by contrast, a difference emerged. In the whole trial cohort, the treatment group had only 9 percent less accumulation than placebo on a composite tau PET measure, ditto in frontal cortex, with neither change statistically significant. Rapid clearers, however, had 33 percent less tangle growth on the composite measure, 44 percent less in lateral temporal regions, and 41 percent less in parietal cortex. There was also a trend toward slowing in the frontal cortex, with 29 percent less growth (see image above).
Shcherbinin called this “conceptually analogous” to the tau PET effect seen in Phase 2, where accumulation slowed between 32 to 59 percent in lateral temporal, parietal, and frontal lobes. In Phase 2 as well, people who became amyloid-negative benefitted the most (Mar 2021 conference news).
In Phase 3, it appeared that the lower a person’s amyloid load was by one year, the more that person’s tangle growth slowed, with a weak correlation of r=0.2 for the cohort. Lower plaque load at one year also associated with slower cognitive decline, though that relationship was weaker still, at r=0.1. To Shcherbinin's mind, the findings imply that plaque needs to be absent for a few months before tangle growth starts to slow.
Others at CTAD joined the chorus of the benefits of complete plaque removal. John O’Gorman of Biogen showed a post hoc analysis of open-label extension data from the Phase 3 Emerge and Engage trials of aducanumab. In their amyloid PET substudy, the researchers separated those who had cleared the amyloid positivity threshold of 20.2 centiloids by the end of the 18-month study from those who had not. After a year of OLE aducanumab, the 41 people in the amyloid-negative group had slid about a point less on the CDR-SB than had the 99 who were amyloid-positive at the trial’s end. Effects were similar on other outcomes, with about 1.5 points less decline on the MMSE, three on the ADAS-Cog13, and two on the ADCS-ADL-MCI. The findings again point to cognition improving months after plaque removal. O’Gorman cautioned that sample sizes were small, hence subject to bias.
Delayed Cognitive Benefit?
In toto, learnings from immunotherapy trials thus far imply that a person needs to be amyloid-negative for months before they get better. At CTAD, Paul Delmar of Roche presented a meta-analysis of eight immunotherapy trials that supports this. The study comprised Phase 3 aducanumab and lecanemab, and Phase 2 and 3 donanemab and gantenerumab studies. Delmar wanted to know what factors correlated best with efficacy, and when. Prime suspects were amount of amyloid removed, final load, and percentage of participants who became amyloid-negative. For each, Delmar considered two time points: the end of the trial, and a year before the end.
The amount of plaque removed turned out to be a poor measure of efficacy. For example, both the Clarity trial of lecanemab and the Graduate trials of gantenerumab cleared around 60 centiloids, yet the former slowed decline on the CDR-SB by 27 percent, the latter by 7.
The best measure? Plaque load a year before the trial end. This measure correlated most strongly with the final CDR-SB score, with a Spearman coefficient of r=0.85. Similarly, the percentage of amyloid-negative participants a year before the trial end performed well, with a correlation of 0.70. Both were more predictive than amyloid load or negativity at the end of a trial, again highlighting that cognitive benefits lag behind amyloid removal.
Meanwhile, Guoqiao Wang of Washington University, St. Louis, discussed data from the Dominantly Inherited Alzheimer Network’s secondary prevention trial of gantenerumab, which began in 2014. Although the trial was negative, gantenerumab normalized biomarkers in this population (Feb 2020 news; Apr 2020 conference news). The study enrolled people at various stages of autosomal-dominant AD, where some were already symptomatic but most were not, hence treatment effects varied from person to person. In particular, because gantenerumab dosing started low, and mutation carriers deposit plaque quickly, some people continued to accumulate amyloid on drug.
To find out if any group had a cognitive benefit, Wang divided the 52 people taking gantenerumab into the 20 who responded with lower plaque, the 18 with no change, and the 14 with continuing amyloid deposition. These three groups did not differ from each other at baseline in disease stage, amyloid load, or cognitive scores, he noted.
After six years of treatment, the responder group had declined 47 percent less on the CDR-SB than had the continuing deposition group. Similarly, other cognitive tests showed between 32 and 57 percent less slippage. Curiously, the no-growth amyloid group had the least cognitive decline of all, as well as the least change on MRI biomarkers, behaving much like non-progressors seen in other Alzheimer’s trials. Cerebrospinal fluid p-tau181 and total tau stayed relatively stable in the no-growth and amyloid-growth groups, and dropped in the amyloid-lowering group.
The size of therapeutic benefit in the amyloid-lowering group was similar to that seen in the positive trials of lecanemab and donanemab, Wang noted. He believes the findings represent a step toward establishing plaque removal as a surrogate endpoint for trials.

Never Mind APOE? A meta-analysis of amyloid immunotherapy trials found no consistent difference in the cognitive benefit between APOE4 carriers and noncarriers. [Courtesy of Eli Lilly.]
APOE4 Carriers: Same Small Benefit, Might Need Earlier Treatment
Does a person's APOE genotype affect how much immunotherapy helps them? Intuitively, the assumption might be “yes,” but previous studies generated mixed results, with APOE4 carriers sometimes doing better and sometimes worse than noncarriers. Indeed, in Boston, Lilly’s Cynthia Evans made a case for genotype having no overall effect. First, she analyzed Trailblazer-Alz2 data, where E4 carriers made up 72 percent of the cohort. Carriers and noncarriers benefitted nearly identically on all clinical tests, both in the primary analysis population of people with low-to-intermediate tangle loads, and in the full population that included those with more baseline tangles. The APOE genotypes also cleared plaque at the same rate—after taking into account more treatment pauses due to ARIA in E4 carriers, that is.
Next, Evans presented a meta-analysis of Phase 2 and 3 donanemab trials along with Phase 3 aducanumab and lecanemab trials. Despite variation in individual trials—for example, noncarriers fared worse on drug than placebo in certain trials—there was no consistent difference overall between carriers and noncarriers on the CDR-SB or ADAS-Cog, Evans reported (see image above).
What is different? In Trailblazer-Alz2, APOE4 carriers were two years younger than noncarriers, but still had the same plaque load at baseline. This agrees with previous work showing that plaque accumulates at younger ages in carriers (Reiman et al., 2020). In addition, APOE4 carriers in Trailblazer-Alz2 trended toward more tangles, with a baseline tau PET SUVR of 1.22, versus 1.20 in noncarriers.
A recent paper sheds light on this relationship between APOE4 and tangles. Researchers led by Nicolai Franzmeier of Ludwig Maximilian University in Munich analyzed amyloid and tau PET scans from two observational studies, ADNI and Avid-A05, Lilly’s tau imaging study (Pontecorvo et al., 2017). The former comprised 237 participants, the latter 130. In ADNI, 45 percent were E4 carriers, in Avid-A05, 35 percent. Participants ranged from cognitively healthy to mild cognitive impairment.
First author Anna Steward compared longitudinal tau PET scans done 1.5 to two years apart. In both studies, amyloid-positive E4 carriers had faster cortical tangle spreading, at lower plaque loads, than did noncarriers. The speed at which tangles accumulated started diverging between the groups at plaque loads as low as 12 to 15 centiloids, when amyloid PET scans are still considered negative.
This means APOE4 might lower the threshold at which “Aβ starts bothering tau” (Nov 2023 conference news). If so, this would also mean that immunotherapy should start earlier in E4 carriers than noncarriers, the authors concluded. APOE4 was previously found to promote tau pathology in animal models (Sep 2017 news).
Getting Under Your Skin
Most efficacy data so far comes from trials of antibodies infused into people's veins. However, companies are investigating injection under the skin as an easier, more scalable delivery method. How do the two compare? Quite well, according to Eisai’s Michael Irizarry. In Boston, he showed interim data from the company’s subcutaneous lecanemab formulation, which was added to the open-label extension of the Phase 3 Clarity trial.
Out of 394 OLE participants, 322 had previously gotten IV lecanemab. The other 72 were new to the drug, either because they had been on placebo, or because they enrolled directly into the OLE. Both groups started treatment at about 77 centiloids. Participants received 720 mg of lecanemab weekly, administered as two doses. The trial used two methods of getting the antibody in, auto-injector pens and syringes filled from a vial. They performed about the same, Irizarry said.
At an interim, six-month time point, subcutaneous dosing resulted in 11 percent higher exposure in blood than did IV, Irizarry reported. Comparing people new to lecanemab with the results from Clarity, it also removed 14 percent more amyloid, in keeping with the higher exposure. The trial will continue to 12 months.
Subcutaneous safety was similar to that of IV lecanemab, with local injection reactions such as redness and swelling in 8 to 15 percent of people, few systemic reactions, and no skin rashes. Alas, subcutaneous lecanemab did appear to produce more ARIA than the IV version, 17 versus 13 percent ARIA-E, and 22 versus 17 percent ARIA-H, also in keeping with the higher exposure.
Notably, dosing made lecanemab blood levels more stable, without the high peak or drop seen with IV administration. For IV dosing, peak exposure had correlated with ARIA-E, leading researchers to hope that lowering this would lessen ARIA. However, for SC lecanemab thus far, total exposure correlated with ARIA-E, and overall rates were comparable to IV.
Eisai has said it will submit a Biologics License Application to the U.S. Food and Drug Administration for the subcutaneous formulation by March of 2024. It is likely other drug makers will follow suit with their own SC formulations, hence fewer people may need to travel to infusion centers for amyloid immunotherapy in the future.—Madolyn Bowman Rogers
References
Therapeutics Citations
News Citations
- Donanemab Data Anchors Upbeat AAIC
- Biomarkers and Efficacy: Not (Yet?) a Perfect Union
- Donanemab Confirms: Clearing Plaques Slows Decline—By a Bit
- Topline Result for First DIAN-TU Clinical Trial: Negative on Primary
- In DIAN-TU, Gantenerumab Brings Down Tau. By a Lot. Open Extension Planned
- Treat Before ‘Aβ Bothers Tau,’ Scientists Say at CTAD
- ApoE4 Makes All Things Tau Worse, From Beginning to End
Paper Citations
- Reiman EM, Arboleda-Velasquez JF, Quiroz YT, Huentelman MJ, Beach TG, Caselli RJ, Chen Y, Su Y, Myers AJ, Hardy J, Paul Vonsattel J, Younkin SG, Bennett DA, De Jager PL, Larson EB, Crane PK, Keene CD, Kamboh MI, Kofler JK, Duque L, Gilbert JR, Gwirtsman HE, Buxbaum JD, Dickson DW, Frosch MP, Ghetti BF, Lunetta KL, Wang LS, Hyman BT, Kukull WA, Foroud T, Haines JL, Mayeux RP, Pericak-Vance MA, Schneider JA, Trojanowski JQ, Farrer LA, Schellenberg GD, Beecham GW, Montine TJ, Jun GR, Alzheimer’s Disease Genetics Consortium. Exceptionally low likelihood of Alzheimer's dementia in APOE2 homozygotes from a 5,000-person neuropathological study. Nat Commun. 2020 Feb 3;11(1):667. PubMed.
- Pontecorvo MJ, Devous MD Sr, Navitsky M, Lu M, Salloway S, Schaerf FW, Jennings D, Arora AK, McGeehan A, Lim NC, Xiong H, Joshi AD, Siderowf A, Mintun MA, 18F-AV-1451-A05 investigators. Relationships between flortaucipir PET tau binding and amyloid burden, clinical diagnosis, age and cognition. Brain. 2017 Mar 1;140(3):748-763. PubMed.
Further Reading
Primary Papers
- Steward A, Biel D, Dewenter A, Roemer S, Wagner F, Dehsarvi A, Rathore S, Otero Svaldi D, Higgins I, Brendel M, Dichgans M, Shcherbinin S, Ewers M, Franzmeier N. ApoE4 and Connectivity-Mediated Spreading of Tau Pathology at Lower Amyloid Levels. JAMA Neurol. 2023 Dec 1;80(12):1295-1306. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
Stanford University
While it is encouraging to see alternative hypotheses being generated from post hoc data analyses, I'm not certain the field has fully come to grips with the lack of correlation between amount of amyloid removal and clinical efficacy. This is certainly what one would expect of a surrogate biomarker deemed "likely to predict a clinical benefit" by the FDA. We almost never see, either in papers or presentations, scatterplots showing within trial correlations between amyloid plaque removal and clinical outcome across individuals. What is frequently shown, instead, is a correlation plot across trials suggesting that those trials that achieved a greater amount of amyloid removal tend to have better clinical outcomes. The only within trial data we could obtain (from the two Phase 3 aducanumab studies) show no significant correlation between amyloid removal and change in CDR-SB (Figure 1B in the paper cited below).
Furthermore, just as there is a correlation between amyloid removal and clinical response across trials, we have shown a correlation between percentage of subjects with ARIA-E and clinical response across trials (Figure 2 in the paper cited below). This raises the concerning possibility that functional unblinding due to ARIA is driving some or all of the clinical effect in these studies. Given the arguable clinical relevance of the outcome data reported, even some contribution from a functional unblinding/placebo effect would be worrisome. The utter lack of movement in the tau PET measures in the donanemab study (which had the largest effect on CDR-SB and had the largest reported tau PET sub-study) would be consistent with such a non-biologically-mediated effect on clinical outcome measures.
It is certainly possible that the correlation between ARIA and clinical outcomes across trials reflects some co-linearity, across trials, between amyloid removal and ARIA. The pharmaceutical companies could, easily, shed light on this topic in several different ways. Providing spaghetti plots of each subject's longitudinal course with time stamps indicating which subjects had ARIA and when would be incredibly informative. Is there a presumably non-biological, post-ARIA "bump" in CDR-SB that would support a functional unblinding/placebo effect? It would also be helpful, in each trial, to compare participants in the active treatment arm who did have ARIA with participants in the active treatment arm who did not have ARIA, matched for relevant variables like amount of amyloid removed (or speed of removal), age, sex, and APOE4 dose. If ARIA is not inflating clinical outcomes these two groups should have similar clinical responses. As discussed in our commentary, the sensitivity analyses designed to address the potential impact of ARIA on functional unblinding in the lecanemab and donanemab studies are hobbled by the greater risk of ARIA in APOE4 carriers.
The "speed of amyloid removal" hypothesis strikes me as entirely plausible but it has been generated, appropriately, from post hoc analyses. The field would advance more quickly if we had a better understanding of within-trial associations between amyloid removal, ARIA and outcomes.
References:
Digma LA, Winer JR, Greicius MD. Substantial Doubt Remains about the Efficacy of Anti-Amyloid Antibodies. arXiv:2310.15456 [q-bio.TO], November 19, 2023 Cornell University, Quantitative Biology
Make a Comment
To make a comment you must login or register.