Las Vegas: Can Collaboration Speed Drug Discovery for FTD?
Quick Links
Given their complex pathophysiology and bewildering array of clinical symptoms, frontotemporal dementias (FTDs) have long stymied scientists’ attempts to model these disorders at the lab bench and to test drugs against them. However, at the "Frontotemporal Dementia: The Next Therapeutic Frontier" meeting held 25-26 March 2011 in Las Vegas, stakeholders from academia, pharma, nonprofits, and government agencies heard about a recent surge of developments that suggest the tide may be turning (see Part 2). “There are many potential approaches, and oodles and oodles of models. You really don’t know how to pick and choose,” Michael Gold of Allon Therapeutics, Vancouver, Canada, told ARF. And when it comes to testing disease-modifying compounds for disorders that are 200 times less prevalent than Alzheimer’s, companies need to be choosy about which ones they push into the clinical pipeline. “We don’t have the luxury of doing a lot of trials,” said Adam Boxer, University of California, San Francisco. “We have to be sure a compound is a good bet going into a trial.” Boxer chairs the steering committee of the FTD Treatment Study Group (FTSG), which includes Gold and four others (see Part 2). The group formed about a year ago to accelerate drug development for these disorders, and sponsored the recent conference at the Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas.
Other rare disorders face similar predicaments, and independent nonprofit organizations have stepped in by facilitating collaboration among academia, industry, and government bodies. In Las Vegas, attendees heard about several of these initiatives and weighed in on similar efforts brewing for FTD.
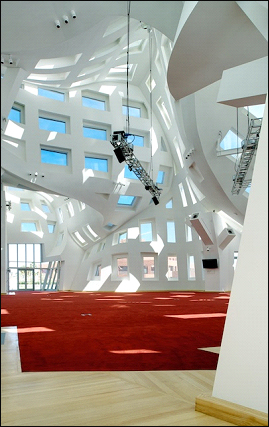
The event center of the Cleveland Clinic Lou Ruvo Center for Brain Health receives natural lighting from 199 uniquely shaped windows. This space hosted the first independent meeting of the Frontotemporal Dementia Treatment Study Group, held 25-26 March 2011 in Las Vegas. Image credit: Matt Carbone Photography
With a single identified gene mutation causing the disorder, Dan van Kammen hailed Huntington’s disease as a poster child for drug development in rare diseases. Recently retired from the Cure Huntington’s Disease Initiative (CHDI) Foundation, Inc., van Kammen described how CHDI has worked with biotech and pharma companies to develop a pipeline of therapeutic targets. As a virtual biotech, CHDI has standardized HD animal models and cell assays for evaluating potential therapeutic approaches, and rallied scientists worldwide to share data and form collaborations with the shared mission of speeding HD drug development.
To make this happen, CHDI has created a website where researchers can exchange ideas and learn the latest on HD drug discovery efforts. In an effort to impart some standardization and comparability on the individualized nature of academic datasets, the foundation has developed a scorecard for assessing mechanistic data and “druggability” of some 800 molecules claimed to be involved in HD. This is annotated on the website, which is open to registered users.
More recently, CHDI worked with the Public Library of Science to launch PLoS Currents: Huntington Disease, a peer-reviewed journal that processes manuscripts rapidly and, importantly, accepts negative data that might otherwise never see the light of day. This may prevent scientists from wasting time and money on unsuccessful research paths, van Kammen noted. “Research foundations today have an important role in serving as a safe meeting ground for academia, NIH, and industry to address issues important for drug development that are unlikely to be addressed by any party alone,” van Kammen said.
Besides expressing support for those efforts, National Institute of Neurological Disorders and Stroke (NINDS) program director Margaret Sutherland discussed the induced pluripotent stem cell initiative funded by NINDS. It aims to create fibroblast iPS lines with known mutations for Huntington’s, Parkinson’s, or amyotrophic lateral sclerosis (ALS), and make the cells available to scientists through biobanking at Coriell Institute for Medical Research in Camden, New Jersey (see ARF iPS story). The iPS consortia are “an example of where government, academics, non-government organizations, and pharma can come together to work toward a common goal,” Sutherland said. “It works because it is a noncompetitive space. We all recognize similar limitations.”
Steve Perrin heads the ALS Therapy Development Institute (ALS TDI), a nonprofit organization in Cambridge, Massachusetts. There, some 30 scientists, mostly from pharma, plug away with a singular objective, that is, developing drugs to stop amyotrophic lateral sclerosis as soon as possible. In Las Vegas, Perrin discussed the importance of rigorous preclinical study design, the relative lack of which in the past he sees as the reason many drugs that look fantastic in mice later flop in human trials. He used as examples three compounds (celecoxib, minocycline, and lithium) with preclinical data published in high-tier journals that failed to translate in the clinic. All ended up in Phase 3 trials, but would have never reached human testing had the preclinical studies been held to more stringent standards, Perrin said (see also Alzforum Webinar).
Among the standards Perrin mentioned were these: making sure mice are dying of ALS instead of something else, genotyping to check the transgene copy number in transgenic animals, examining outcomes separately in male and female mice. Had such guidelines been used, none of these three compounds would have helped ALS model mice nearly as much as, for example, blocking interactions between CD40 and its ligand CD40L, a separate potential therapeutic approach identified in a recent analysis by Perrin and colleagues (ARF related news story on Lincecum et al., 2010; stay tuned for upcoming Alzforum Webinar with Perrin).
Whereas ALS TDI takes a brick-and-mortar approach to fighting ALS, the Coalition Against Major Diseases (CAMD) works in large part as a distributed organization coordinating projects for AD and PD. An initiative of the Critical Path Institute, CAMD has an online data repository with information from some 4,000 AD patients in 11 industry-sponsored clinical trials. Last November, CAMD gathered representatives from academia, industry, funding, policy, and regulatory authorities in Washington, DC, to discuss ways to reform AD drug trials (see ARF related series). In Las Vegas, Marc Cantillon, CAMD’s executive director, stressed the importance of formal legal agreements in making these collaborations work. The contracts not only compel all parties to share data, but also spell out exactly what will be done with the intellectual property generated by the joint research.
CAMD showed that “companies are willing to part with proprietary information,” Gold told ARF. “You can get big companies to contractually agree to share data with a neutral third party.” Gold challenged the Lou Ruvo audience to consider a similar arrangement for accelerating FTD drug discovery. “We are far behind the AD field in terms of how we are organized, how we share data, and how we do clinical trials. It is high time that we start to focus and customize the treatments,” he said. “The fundamental question is, How do you pick which compounds to move into clinical trials?”
Such issues are critical for tauopathies, which by virtue of their lower prevalence and heterogeneity will have much smaller markets. A smaller potential return limits companies’ willingness to invest. “With low prevalence conditions, you have multiple resource constraints,” Gold said. “If you are talking about disease-modifying compounds…these will likely entail long studies. We need to think more carefully about what molecules we move into such expensive studies, and what strength of evidence is required.”
To help the field make these decisions, Gold laid out a “collaborative competition” model, whereby only the most promising compounds would get tested in the most relevant models. “We are looking for a rational transaction that optimizes the outcome,” he said. Not long ago, such transactions were simpler because they were mostly unidirectional—Party A (academic lab) developed a model that could be used to test compounds developed by Party B (company). Nowadays, the lines are blurring as companies make models and universities try their hand at compound screening and medicinal chemistry. “Party A or B may be either a pharma company or an academic center,” Gold said. “Intellectual property issues are more convoluted.”
In the framework Gold envisions, all parties would sign a contract agreeing to share their data with an FTSG-run “clearinghouse” for FTD drug discovery that would match compounds to models based on a pre-specified scoring procedure. Gold compared this process to those used by the National Resident Matching Program to connect medical school graduates with residency programs, or by the National Collegiate Athletic Association for matching student athletes with schools. The clearinghouse would be funded by all participants, though not necessarily equally by academic labs and companies. “Everybody shares in the risk. Everybody potentially shares in the reward. We need to work together, but at the end of the day, only the best compounds should enter the clinic,” Gold said. Beyond setting licensing terms, the clearinghouse could create and administer patent pools, Gold said, and help arrange cross-licensing across multiple parties—for example, to license a model for the testing of more than one molecule.
In a subsequent presentation, Boxer showed a mock homepage for an FTD website to facilitate the data sharing that would fuel the clearinghouse. The proposed website would serve as a go-to for information on FTD, treatment development, and on the FTD Treatment Study Group. It would have pages describing the various animal and cellular models—their strengths and weaknesses, genetic tools available, targets that could be tested, studies by other investigators using the model, and so forth. In addition, Boxer said, the website would have a password-protected section where pharma scientists could contribute information on potential therapeutic compounds.
On this, the FTSG has its work cut out. Few pharma scientists spoke up during discussion of the website and clearinghouse ideas. The ones who did, as well as others who spoke with this reporter at the meeting and/or via e-mail afterward, expressed as much hesitation as excitement for these proposals. Susan Abushakra of Elan Corporation, South San Francisco, noted that, in her personal opinion, it would “need an army of lawyers” to get companies to give proprietary data to a shared website they do not control. Another industry scientist said the website is “great for academia” but “would not work with industry.”
However, some pharma companies might be willing to say they have certain data—for example, whether a compound has gone through certain stages of preclinical development, or whether it has been tested in various animal models—without disclosing precisely what the data are, suggested Gerhard Koenig of EnVivo Pharmaceuticals in Watertown, Massachusetts. “That’s one way industry may be able to contribute (to the website),” he said. Another option for industry participation might lie with compounds that are either non-druggable or have no intellectual property protection, Abushakra suggested, “These can be used as probes or tools to characterize the non-clinical models.” Gold stressed that the terms under which data are loaded onto the website would be negotiated and clear to all parties beforehand.
Several attendees articulated the concern that academic researchers are not given proper incentives to do the best drug development studies. “Negative studies don’t get published, and you don’t get rewarded for doing replicative studies that try to confirm the same thing in a variety of different models,” Boxer told ARF. Toward this end, several company directors said a joint website could hold great value as a central repository for preclinical data, both positive and negative. Blair Leavitt of the University of British Columbia, Canada, wondered whether the field needs something like a ClinicalTrials.gov for animal studies. “Negative results have to be brought out,” he said.
Beyond data sharing, a website might drive drug discovery forward by displaying the licensing terms for various models, an industry representative noted. “It would be useful if, up front, institutions with models would work with their legal licensing groups to make terms for academic and industrial use clearly available upon request, and post these on the website,” he wrote. In AD, the Jackson Laboratory’s Alzheimer’s Disease Mouse Model Resource has addressed some of these problems. Led by Mike Sasner at JAX in Bar Harbor, Maine, this project obtains and re-derives desirable mouse models in the field and makes them available for a nominal fee to other investigators. In the process, the resource has gained experience with many of the institutional licensing problems that come up.
As for the proposed clearinghouse, some were concerned it could actually slow drug development. “Committees are not the best way to make decisions in a difficult, evolving field,” one company executive suggested. “Many successful drug hypotheses have been ‘maverick’ ideas that failed to get approval by committees for funding, or support by colleagues in pharma companies. I hope the FTD Treatment Study Group will focus on facilitating vigorous debate rather than act as a gatekeeper.”
On the whole, companies found the meeting packed with new data on FTD preclinical models that could lead to increased pharma interest—but most are not jumping into the fray just yet. “We will continue to watch developments in this evolving area very closely,” wrote Greg Flesher of Avanir Pharmaceuticals, Aliso Viejo, California. “Tau therapies are exciting, but very early and high-risk programs.” A wait-and-see approach is not enough for Jeffrey Cummings, who directs the Lou Ruvo Center in Las Vegas and serves on the FTSG steering committee. “We can have meetings until the next ice age…but if our mission is to accelerate entry of compounds into clinical trials, then we need a different framework that requires exchange of proprietary information,” Cummings said.
In Las Vegas, attendees knocked heads over the pros and cons of various organizational and funding models for the FTD Treatment Study Group, including the possibility of a formal affiliation with the Association for Frontotemporal Degeneration (AFTD). Whatever solution they’ll arrive at, the group knows it wants “to stay focused on drug development for FTD, on getting molecules to the clinic,” Boxer told ARF. The next meeting of the FTD Treatment Study Group will focus on clinical trials and biomarkers, and will likely occur in conjunction with the Clinical Trials on Alzheimer’s Disease Conference, 3-5 November 2011 in San Diego.—Esther Landhuis.
This concludes a three-part series. See also Part 1 and Part 2. See PDF of entire series.
References
News Citations
- Las Vegas: Are Frontotemporal Dementia Models Fit for Pharma?
- In Alzheimer Disease Research, iPS Cells Catch On Slowly
- ALS-TDI Scours Transcriptome, Targets CD40L
- DC: CAMD Convenes Stakeholders to Reform Alzheimer’s Trials
Webinar Citations
Paper Citations
- Lincecum JM, Vieira FG, Wang MZ, Thompson K, De Zutter GS, Kidd J, Moreno A, Sanchez R, Carrion IJ, Levine BA, Al-Nakhala BM, Sullivan SM, Gill A, Perrin S. From transcriptome analysis to therapeutic anti-CD40L treatment in the SOD1 model of amyotrophic lateral sclerosis. Nat Genet. 2010 May;42(5):392-9. PubMed.
Other Citations
External Citations
Further Reading
News
Annotate
To make an annotation you must Login or Register.

Comments
Mithridion, Inc.
The scientific and clinical content of the meeting in Las Vegas was thought provoking. I came away with new insights about FTD. Plus, it provided a tremendous forum to meet leading investigators in the FTD field and to exchange ideas. Just by bringing us together, the FTD Treatment Study Group promises to make a pivotal contribution to accelerating drug development for these devastating diseases. As we heard at the meeting, research progress is accelerating. We are investing more in this disease area.
I think the idea of "pre-competitive” collaboration is good, and the FTD Study Group could play a valuable, facilitative role in this. Being able to collaborate on in vitro and in vivo models could accelerate preclinical drug development and help us get drugs ready for clinical evaluation. We have mechanistic models with good construct validity for FTD, but modeling focal neurodegeneration and outcomes is very challenging. An ongoing dialogue among clinicians, basic researchers, and drug hunters about the validity of models, drug targets, and drug leads is another valuable contribution the FTD Study Group could make.
Make a Comment
To make a comment you must login or register.