217—The Best Phospho-Tau Marker for Alzheimer’s?
Quick Links
A flood of recent data seems to leave little doubt that phospho-tau217 is the better of the soluble tau markers for studying Alzheimer’s disease thus far. At this year’s virtual AAT-AD/PD meeting, Oskar Hansson, Lund University, Sweden, reported that p-tau217 in the CSF correlates more strongly with neurofibrillary tangles and amyloid plaques than does p-tau181 or total tau. CSF p-tau217 climbs higher, and better distinguishes AD from controls and non-AD forms of dementia, as well, said Hansson.
- CSF P-tau217 strongly correlates with plaques and tangles in AD.
- It distinguishes Alzheimer’s from other dementias better than does p-tau181.
- P-tau217 best predicts accumulation of neurofibrillary tangles.
Both 217 and 181 p-tau ticked up in the CSF before tau PET scans became positive, indicating that phosphorylation at these two sites represents a very early response to Aβ. The findings appear in the April 3 Nature Communications and the April 15 Science Advances, the latter paper being delayed due to the coronavirus pandemic.
Separately, in the March 17 Alzheimer’s Research & Therapy, researchers led by Nicolas Barthelémy at Washington University, St. Louis, Audrey Gabelle at Gui de Chauliac Hospital, Montpellier, France, and Sylvain Lehmann, University of Montpellier, reported that of the two phospho-taus, p-tau217 better correlates with amyloid plaques. Almost without exception, people with AD have more of the marker in the brain than anyone else. Hansson thinks p-tau217 will soon take over from p-tau181 as the go-to tau marker for AD. “While the difference [between them] is not huge, it is consistent, so why use a test that is less accurate?” he asked.
Eric McDade, WashU, agreed. “As the authors suggest, with validation in larger cohorts, p-tau217 may become the gold standard as an AD diagnostic test, particularly if this phosphorylation site can be reliably detected in the blood.” (See full comment below.)
These reports come shortly after a paper last month by Barthelémy and colleagues. It detailed how p-tau217 is the first tau species to rise in the CSF of people with autosomal-dominant AD, edging up some 21 years before the expected age of symptom onset (Mar 2020 news). The data in the new batch of papers pertain to sporadic AD.
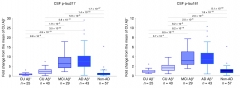
A Better Test. Across the AD spectrum, fold changes in CSF p-tau217 (left) are larger than for p-tau181 (right). [Courtesy of Shorena Janelidze, Nature Communications.]
In Hansson’s group, Shorena Janelidze compared levels of p-tau217 and p-tau181 in CSF samples from the Swedish BioFINDER study. Both tau species were measured on the Meso Scale Discovery platform, using immunoassays developed by Jeffrey Dage at Eli Lilly, Indianapolis. These two-step ELISAs used antibodies specific to p-tau217 and p-tau181 for capture, but the same N-terminal tau antibody for detection; this should reduce between-assay variability, the authors noted. Janelidze measured both isoforms in CSF from 194 volunteers, of whom 184 had had a flortaucipir PET scan for neurofibrillary tangles and 139 a flutemetamol scan for amyloid. The cohort included 65 cognitively normal controls, 29 with Aβ-positive MCI, 43 with AD, and 57 who had non-Alzheimer’s disease dementia.
Levels of both p-tau forms were highly correlated to each other. That said, p-tau217 showed a higher dynamic range across the AD disease spectrum. It rose eightfold in MCI/AD over Aβ-negative normal controls, where p-tau181 was fourfold higher.
Both p-taus correlated with plaques and tangles as per PET. Again, this was stronger for p-tau217, which covered more “area under the curves” for predicting flortaucipir binding at all Braak stages of tau progression. Likewise, the AUCs for predicting abnormal CSF Aβ42 and amyloid PET were 0.910 and 0.827, respectively, for p-tau217, versus 0.890 and 0.799 for p-tau181. Measuring the ratio to total tau improved these AUCs for p-tau217 to 0.914 and 0.871 and for p-tau181 to 0.914 and 0.859. All told, the data indicate that p-tau217 is a more robust marker of underlying AD pathology.
Janelidze found a similar pattern in a second BioFINDER cohort of 330 people comprising normal controls and people with MCI. To corroborate further, the researchers tested CSF from 32 people in Lilly’s EXPEDITION3 trial of solanezumab. Here, too, CSF p-tau217 correlated with flortaucipir binding even more strongly than did p-tau181.
The pattern in BioFINDER also held when p-tau217 and total tau were measured with a different pair of immunoassays developed by Janssen Research and Development, La Jolla, California. Again, p-tau217 better correlated with tau PET and better differentiated AD from other neurodegenerative disorders. “Taken together, these findings suggest that increases in CSF p-tau might reflect AD-related tau hyperphosphorylation rather than only increased production and secretion of tau from cells, and that in AD, changes in soluble tau metabolism affect to a larger extent phosphorylation at Thr217,” write the authors.

Unambiguous? In the Montpellier cohort, mass spectrometry shows that p-tau217 (bottom) is consistently higher in the CSF of people with AD than in the CSF of those with other dementias, some of whom (numbers 1 to 3) had abnormally high p-tau181 (top). [Courtesy of Barthelemy et al., Alzheimer’s Research & Therapy.]
Barthelémy and colleagues reported similar findings among a cohort of 50 clinically well-characterized dementia patients in Montpellier. Mass spec analysis of their CSF indicated a higher dynamic range for p-tau217, much like Hansson and colleagues found. This isoform rose up to sixfold in the AD samples compared with non-AD, whereas the 181 form only rose 1.3-fold. The 10 people with AD had consistently more p-tau217 in their CSF than did 40 people with non-AD dementias. Here again, the 217 isoform performed best, since three of the non-AD samples had p-tau181 levels in the AD range, a recipe for misdiagnosis (see image above).
These researchers also compared CSF phospho-tau isoforms in a cohort of 84 people from the Alzheimer’s Disease Research Center at Wash U. This included 51 Aβ-negative controls and 33 Aβ-positive individuals with mild cognitive impairment or AD. While there was considerable overlap between levels of p-taus in the two groups, p-tau217 was higher in almost all Aβ-positive samples, distinguishing Aβ-positives from -negatives with an AUC of 0.961. For p-tau181 the AUC was 0.785.
P-tau217 also tightly correlated with amyloid PET. “The data obtained show that CSF pT217 is a much more highly specific marker than pT181 for detecting both preclinical and advanced AD,” write the authors.
The data from both groups support the idea that phosphorylation of tau at specific sites is an early and specific response to Aβ toxicity, and that it precedes the formation of neurofibrillary tangles. In his ADPD presentation, Hansson drilled deeper into when in the disease tau gets phosphorylated. Niklas Mattsson and colleagues at Lund compared soluble tau and tangle levels in BioFINDER. Of 131 people studied, 113 had brain amyloid based on their Aβ42/40 ratio in the CSF. They included 40 people who were cognitively normal, 38 with MCI, and 35 with AD. The remaining 18 were amyloid-negative and cognitively normal.
Mattsson found that of the 18 controls, 17 tested negative for soluble CSF tau and tau PET; one person had both high p-tau217 and p-tau181. However, among the Aβ-positive cognitively normal volunteers, there were already signs of tau pathology. Of these 40, nine, 22, and 28 had elevated total tau, p-tau181, and p-tau217, respectively. Still, only one had tangles in the inferior temporal cortex (ITC) as per flortaucipir binding, suggesting that tangles come later.
Analysis of the MCI and AD groups supported this time sequence. Nearly all had elevated p-tau181 and p-tau217, and 73 percent also had elevated total tau. Three-quarters of those with MCI had tangles in the ITC, while everyone with AD did. Tangles had spread to Braak stage V-VI regions in 32 percent of the MCI subjects and 66 percent of the AD patients.
The data indicate that soluble p-tau emerges before tangles. Looking at this a different way, Hansson compared ITC tangle and soluble tau positivity. He used cutoffs of 1.31 SUVR for the former and 152.6 pg/mL and 119.5 pg/mL for p-tau181 and p-tau217, respectively. For half the cohort the markers were concordant, meaning people tested positive for both. When the markers were discordant, it was almost always the phospho-tau that was abnormal. For example, 28 percent of people tested positive for only p-tau217, but only 1 percent tested positive for only tangles. “The data suggest that people move from normal CSF and normal PET, to abnormal CSF and normal PET, and then to abnormal CSF and abnormal PET,” said Hansson.
How does this tie in with Aβ? Hansson showed that p-tau181/217 turn positive before amyloid PET does, while tau PET turns positive after. Again, this puts phosphorylation before tangles in the pathological cascade. In fact, correlating tau PET with amyloid PET, Mattsson and colleagues found that as amyloid rose, tangles only accumulated if people had already tested positive for p-tau181 (they did not look at p-tau217 in this scenario). “This suggests you need p-tau181 to get tangles,” said Hansson. Mattsson agrees. “There is a very strong relationship between amyloid and tau PET, and it is to a very large degree mediated by changes in soluble tau,” he said. Mediation analysis indicated that p-tau217 and p-tau181 explained 82 and 68 percent, respectively, of the Aβ-driven increase in tangles.
Mattsson stressed that this is all still a bit speculative. “To really prove this chain of events, we’d want to block increases in soluble tau and see if that prevents the transition to tau aggregates,” he said. There are hints from human studies. For example, Mattsson found that people with MAPT mutations, who have no Aβ pathology, also have no p-tau181/217 in their CSF even though they do accumulate a different type of tangle than seen in AD.
This suggests Aβ kicks of a specific tau cascade that begins with these phospho forms. Just recently, data from the DIAN-TU trial of gantenerumab showed that this anti-Aβ immunotherapy dramatically reduced levels of soluble total tau and p-tau181 (April 2020 conference news). “This is a very nice way, with an intervention study, to address the cascade we are suggesting,” said Hansson. “The next step would be to see if the treatment reduces the accumulation of tangles.”—Tom Fagan
References
News Citations
- Different CSF Phospho-Taus Match Distinct Changes in Brain Pathology
- In DIAN-TU, Gantenerumab Brings Down Tau. By a Lot. Open Extension Planned
Therapeutics Citations
Further Reading
No Available Further Reading
Primary Papers
- Barthélemy NR, Bateman RJ, Hirtz C, Marin P, Becher F, Sato C, Gabelle A, Lehmann S. Cerebrospinal fluid phospho-tau T217 outperforms T181 as a biomarker for the differential diagnosis of Alzheimer's disease and PET amyloid-positive patient identification. Alzheimers Res Ther. 2020 Mar 17;12(1):26. PubMed.
- Janelidze S, Stomrud E, Smith R, Palmqvist S, Mattsson N, Airey DC, Proctor NK, Chai X, Shcherbinin S, Sims JR, Triana-Baltzer G, Theunis C, Slemmon R, Mercken M, Kolb H, Dage JL, Hansson O. Cerebrospinal fluid p-tau217 performs better than p-tau181 as a biomarker of Alzheimer's disease. Nat Commun. 2020 Apr 3;11(1):1683. PubMed.
- Mattsson-Carlgren N, Andersson E, Janelidze S, Ossenkoppele R, Insel P, Strandberg O, Zetterberg H, Rosen HJ, Rabinovici G, Chai X, Blennow K, Dage JL, Stomrud E, Smith R, Palmqvist S, Hansson O. Aβ deposition is associated with increases in soluble and phosphorylated tau that precede a positive Tau PET in Alzheimer's disease. Sci Adv. 2020 Apr;6(16):eaaz2387. Epub 2020 Apr 15 PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
Washington University
This study by Janelidze et al. is a timely contribution to the field of tau-related AD diagnostics. This study highlights the value of using newer diagnostic platforms to explore additional phosphorylation sites in the CSF of AD. By assessing the association between phosphorylated tau217 (p-tau217) and aggregated amyloid (amyloid PET) and tau (tau PET) at various stages they were able to demonstrate that, compared to p-tau181 and total tau, p-tau217 was better at discriminating AD from non-AD dementias, demonstrated statistically significantly stronger associations with amyloid and tau PET (albeit, relatively small differences), and was reproducible in different cohorts and with different platforms used to measure it. All in all, this study, along with recently published studies assessing p-tau217 levels in the CNS, indicate that this soluble tau-related biomarker is here to stay. Whether it is truly superior to p-tau181 or complementary is not necessarily clear to me. However, given the recently reported performance of plasma p-tau181 in discriminating AD from non-AD cohorts and identifying the presence of elevated tau PET levels reported by these authors in this same cohort (Janelidze et al., 2020), it is unfortunate that a comparison between the CSF p-tau217 and plasma p-tau181 was not performed in this work.
These results strongly support those from our recently published study from the DIAN cohort as well as a very similar publication this month from an American and French cohort using a quantitative mass spectrometry method in demonstrating both the very strong association of p-tau217 with amyloid pathology and as a specific biomarker for AD-related dementia (Mar 2010 news on Barthelemy et al., 2020; Barthelemy et al., 2020) Moreover, in the current work the authors compared two different ELISA-based methods for measuring p-tau271 and found comparable results. Given that the previous studies measuring p-tau217 employed mass spectrometry and had largely similar conclusions, overall, this suggests that increased level of p-tau217 in the CSF is a robust marker for AD. As the authors suggest, with validation in larger cohorts, p-tau217 may become the gold standard as an AD diagnostic test, particularly if this phosphorylation site can be reliably detected in the blood.
References:
Barthélemy NR, Li Y, Joseph-Mathurin N, Gordon BA, Hassenstab J, Benzinger TL, Buckles V, Fagan AM, Perrin RJ, Goate AM, Morris JC, Karch CM, Xiong C, Allegri R, Mendez PC, Berman SB, Ikeuchi T, Mori H, Shimada H, Shoji M, Suzuki K, Noble J, Farlow M, Chhatwal J, Graff-Radford NR, Salloway S, Schofield PR, Masters CL, Martins RN, O'Connor A, Fox NC, Levin J, Jucker M, Gabelle A, Lehmann S, Sato C, Bateman RJ, McDade E, Dominantly Inherited Alzheimer Network. A soluble phosphorylated tau signature links tau, amyloid and the evolution of stages of dominantly inherited Alzheimer's disease. Nat Med. 2020 Mar;26(3):398-407. Epub 2020 Mar 11 PubMed.
Make a Comment
To make a comment you must login or register.