Lancet Commission’s Dementia Hit List Adds Alcohol, Pollution, TBI
Quick Links
At this year’s virtual Alzheimer’s Association International Conference, researchers presented an update to “Dementia prevention, intervention, and care,” the 2017 report commissioned by The Lancet. Published July 30, the new report identifies three additional modifiable risk factors for dementia, bringing the total to 12. Excessive alcohol consumption, air pollution, and traumatic brain injury cause 6 percent of all dementia cases, according to the international panel of experts led by Gill Livingston at University College London. In total, 40 percent of dementia can be prevented, the panel concludes, up from its 2017 estimate of 35 percent.
- New life-course model predicts 40 percent of dementia is preventable.
- Issues pleas to policy makers—and all people.
- Recommends 14 strategies for dementia risk reduction.
The panel revised slightly downward the risk that stems from low-quality education. Also new this year, the report addresses the risk COVID-19 poses to people who already have dementia.
The report’s 28 authors hail from Australia, Europe, India, Israel, Nigeria, and North America. They include clinicians, psychiatrists, epidemiologists, gerontologists, and public health experts. They reviewed and updated the work of the 2017 commission, which was convened to spotlight immediate opportunities for preventing dementia or improving care.
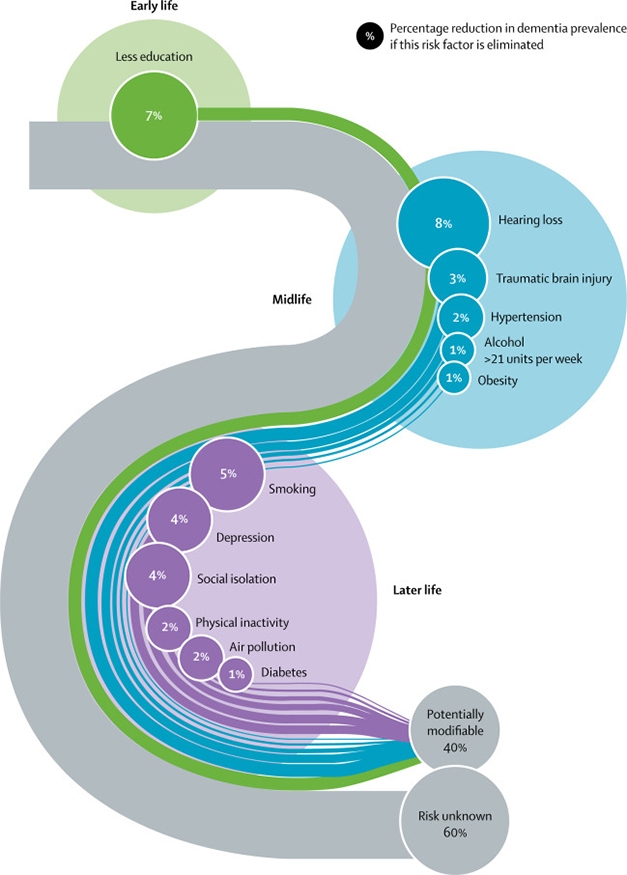
Life Course. This updated model stages 12 modifiable risk factors that together cause 40 percent of dementia cases. Traumatic brain injury, excess alcohol, and air pollution are the new additions. Numbers denote the fraction of the total prevalence attributed to each factor. [Courtesy of Livingston et al., Lancet 2020.]
The 2020 commission’s conclusions come from extensive literature review and meta analyses, including three new studies on alcohol consumption, four on traumatic brain injury, and one study of all-cause air pollution and all-cause dementia among more than 2 million people, average age 67, living in Canada.
According to the report, more than 21 units of alcohol per week is bad news for the brain. Alas, for anyone who still thinks—as scientists have said for years—that what is casually referred to as moderate drinking is good for you, consider this: The report defines a unit as 10 mL of pure alcohol, not a single alcoholic drink. In the U.S., a 12 oz beer at 5 percent alcohol contains 1.775 units, while a large glass of 12 percent wine contains about three units. Hence, two “drinks” per day increase a person’s risk of dementia. A recent French study of more than 31 million people who had been discharged from the hospital concluded that heavy drinking or alcohol dependence tripled a person’s risk for dementia (Feb 2018 news).
Traumatic brain injury, which can be as mild as a concussion or as severe as a skull fracture, increases a person’s risk for dementia by 80 percent, according to the report. TBIs typically come from car and bicycle accidents, sports injuries, military conflicts, or simple falls. TBI accounts for 3.4 percent of all dementia cases. Pollution accounts for 1.1 percent, but this may be higher in low-income communities. All types of air pollutant, including those from traffic and residential heating, have been associated with increased dementia incidence (May 2020 news).
In sum, the panel delivered eight messages for policy-makers and individuals, and recommended 14 strategies for reducing dementia risk (see box below).
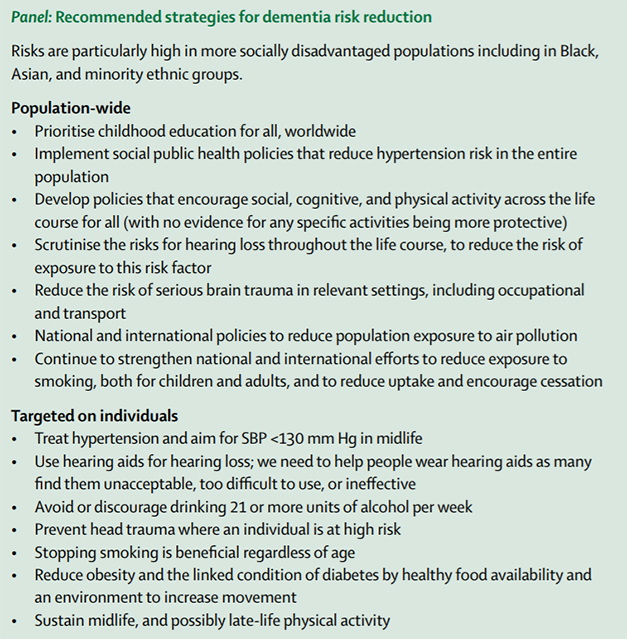
Calling for an ambitious approach to dementia prevention, the scientists note inequalities that put certain groups at higher risk, and warn of a growing dementia incidence confronted by low- and middle-income countries.
Regarding COVID-19, the authors acknowledge that people with dementia are particularly vulnerable because of their age, co-morbidities, and difficulty keeping physical distance. They calculated that in nursing homes, people with dementia were 70 percent more likely to die if they contracted the virus than were residents without dementia. Even so, prevention and treatment strategies, such as isolating patients or transferring them to another location or hospital, can accelerate their decline. The commission recommends vigilant use of personal protective equipment and hygiene for staff, regular SARS-COV2 testing, and making oxygen available for patients who catch the virus but do not want to be transferred to a hospital.
The panel argues for a holistic approach to care, including management of neuropsychiatric symptoms. A holistic approach includes spotting and helping distressed caregivers to alleviate their anxiety, depression, and exhaustion. “I think the caregiving field is a pretty barren area of study, and the Lancet Commission report offers us a way forward,” commission panelist Eric Larson, Kaiser Permanente Washington Health Research Institute, Seattle, told Alzforum.—Tom Fagan
References
News Citations
Further Reading
No Available Further Reading
Primary Papers
- Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, Brayne C, Burns A, Cohen-Mansfield J, Cooper C, Costafreda SG, Dias A, Fox N, Gitlin LN, Howard R, Kales HC, Kivimäki M, Larson EB, Ogunniyi A, Orgeta V, Ritchie K, Rockwood K, Sampson EL, Samus Q, Schneider LS, Selbæk G, Teri L, Mukadam N. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020 Aug 8;396(10248):413-446. Epub 2020 Jul 30 PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.