Exercise Linked to Less Pathology, Better Function in Familial AD
Quick Links
People with autosomal-dominant mutations in APP or presenilin genes develop early onset Alzheimer’s disease. Could a healthy lifestyle mitigate this genetic misfortune? A new study indicates that it may. A cross-sectional study of participants in the Dominantly Inherited Alzheimer Disease Network (DIAN) suggests that higher levels of physical activity associate with better cognitive performance, and less amyloid in the brain. The results are consistent with findings in sporadic AD, and suggest that exercise also benefits people with genetically driven disease. The study, led by Stephan Müller and Christoph Laske of the University of Tübingen in Germany, appeared September 25 in Alzheimer’s & Dementia.
- Exercise staves off dementia in the elderly, but what about people with early onset AD?
- In familial cases, physical activity correlated with better cognition and less disease pathology.
- The study does not establish cause and effect.
The study is the first report of an association between self-reported physical activity and cognitive status in patients with familial Alzheimer’s disease, wrote Antonio Muscari, University of Bologna, Italy, in an email to Alzforum. He stressed that the study shows association, not necessarily causation. “Still, this paper favors the idea that physical activity may be considered an important therapeutic tool for patients at risk of cognitive decline, including those with autosomal-dominant AD,” Muscari said.
The findings may have implications for late-onset, idiopathic AD as well. Studies in familial AD may help us understand what happens in sporadic disease, said Belinda Brown, Murdoch University, Perth, Australia. “By utilizing data from the DIAN families we can evaluate the role physical activity plays in reducing Alzheimer’s disease risk and progression in people who are destined to accumulate amyloid at an early age; thus they provide an excellent model for this type of research,” she wrote to Alzforum.
It has long been known that regular exercise staves off age-related cognitive decline, but the effects of physical activity on amyloid load have been less clear (Mar 2016 news). A small study indicated that exercise slowed amyloid accumulation in presymptomatic AD mutation carriers who already had some amyloid in the brain (Brown et al., 2017). To expand on that study, Müller and colleagues drew on data tallying physical activity, cognitive performance, and biomarkers of amyloid load at baseline among 224 DIAN participants who carry familial AD mutations and 148 healthy, age-matched noncarriers. The carriers averaged 38 years old and spanned the course of the disease, including both asymptomatic and symptomatic volunteers. Participants reported the amount of time they spent over the preceding year doing any of 10 different activities, including walking, cycling, or tennis. A family member or friend corroborated the self-reports. On average, both mutation carriers and noncarriers spent an impressive five hours per week exercising. Among carriers, levels of physical activity were lower in those who were closer to their expected age of disease onset.
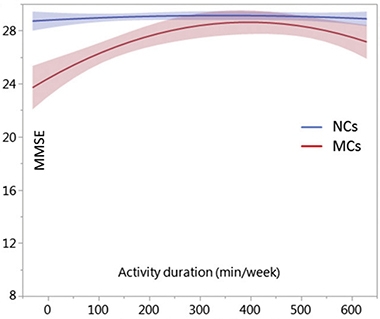
Peak Performance.
In familial AD mutation carriers (red line), a complex dose response exists between physical activity and cognition. Age-matched noncarriers (blue) hold steady at all levels of exercise. [From Müller et al., Alzheimer’s & Dementia, 2018.]
Among the mutation carriers, the researchers identified a complex dose response whereby up to about 6.5 hours per week, more exercise associated with better scores on the Mini Mental State Exam (MMSE) and on the Clinical Dementia Rating scale sum of boxes (CDR-sb). At this level of exercise, MMSE scores approached those of age-matched noncarriers. Above about eight hours of exercise per week, MMSE declined. The CDR-sb followed a similar pattern. Exercise did not relate to cognitive scores in healthy noncarriers.
To delve deeper, Müller divided the mutation carriers into high-activity and low-activity groups, using 2.5 hours per week as the cutoff value. This is the amount of exercise recommended by the World Health Organization, and was achieved by 70 percent of the mutation carriers. On average, the high-activity group was four years younger and hence further from their predicted disease onset than the low-activity group. Perhaps not surprisingly, the high-activity group scored significantly better on the MMSE, CDR global, and CDR-sb than the low-activity group. They also had higher CSF biomarker Aβ1-42, and lower CSF total tau and phospho-tau, all indicative of less AD pathology. Global PiB uptake, a measure of brain amyloid, was slightly lower in the more active group, but the difference was not statistically significant.
When Müller used linear regression to model changes over time, correcting for age and time to disease onset, exercise still appeared to have benefits. Those exercising more had better cognitive function relative to their estimated year to onset (EYO) of dementia than did those who exercised less. At the time when symptoms were predicted to start, the more active group scored 3.4 points better on the MMSE and they reached the CSD-sb cutoff for mild dementia 15 years later than the less-active group. Along with an apparent slowing of cognitive decline, modeled trajectories of CSF total tau and the total tau/Aβ1-42 ratio were attenuated in the high activity group, indicative of less tau and Aβ pathology.
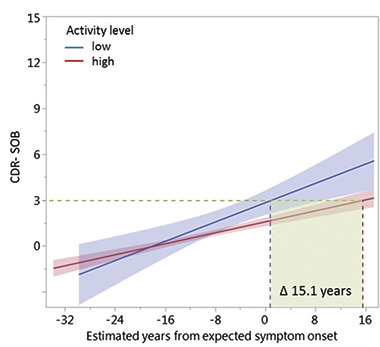
Benefit of Exercise.
Cross-sectional data indicates CDR-SOB scores worsen more gradually in those who are highly active, translating into a 15.1-year lag in reaching the threshold for mild dementia. [From Müller et al., Alzheimer’s & Dementia, 2018.]
Laske was surprised exercise had such a strong effect. “In familial AD, we suppose that the genes are the main drivers, and we didn’t expect that a lifestyle intervention, such as physical activity, could have such strong effects,” he told Alzforum.
Nonetheless, the authors and several commentators cautioned that the data do not prove cause and effect. “With cross-sectional data, we cannot clearly say if higher physical activity is the reason for better cognition, or if better cognition is associated with higher activity,” Laske said. Definitively nailing the effect of exercise will take true longitudinal data, said Laske. In the DIAN study, many participants have by now accumulated five to six years of follow-up data, and Laske is in the process of analyzing those trajectories. Other ADAD cohorts are also collecting information on exercise, with plans to examine the impact of physical activity, wrote Jessica Langbaum of Banner Health Institute, Phoenix, Arizona, in an email to Alzforum (see complete comment below).
“The paper is interesting and is consistent with a lot of other research that indicates a protective association between exercise and the risk of AD, dementia, and cognitive performance,” wrote Eric Larson, Kaiser Permanente Washington Health Research Institute, Seattle, in an email to Alzforum. Larson noted the participants are not typical of the population as a whole, since less than 50 percent of U.S. adults get the recommended 150 minutes of physical activity per week.
Mark Mattson, National Institute of Aging in Bethesda, Maryland thinks the results call for an intervention trial of exercise in familial AD. “It would be good to see if you could actually delay the onset in people who know they would get AD,” he said. He’d also like to see analysis of potential covariates: Perhaps people who exercise more have lower body mass and better glucose control, both of which reduce AD risk, he said.—Pat McCaffrey
References
News Citations
Paper Citations
- Brown BM, Sohrabi HR, Taddei K, Gardener SL, Rainey-Smith SR, Peiffer JJ, Xiong C, Fagan AM, Benzinger T, Buckles V, Erickson KI, Clarnette R, Shah T, Masters CL, Weiner M, Cairns N, Rossor M, Graff-Radford NR, Salloway S, Vöglein J, Laske C, Noble J, Schofield PR, Bateman RJ, Morris JC, Martins RN, Dominantly Inherited Alzheimer Network. Habitual exercise levels are associated with cerebral amyloid load in presymptomatic autosomal dominant Alzheimer's disease. Alzheimers Dement. 2017 Nov;13(11):1197-1206. Epub 2017 May 11 PubMed.
Further Reading
No Available Further Reading
Primary Papers
- Müller S, Preische O, Sohrabi HR, Gräber S, Jucker M, Ringman JM, Martins RN, McDade E, Schofield PR, Ghetti B, Rossor M, Fox NN, Graff-Radford NR, Levin J, Danek A, Vöglein J, Salloway S, Xiong C, Benzinger T, Buckles V, Masters CL, Sperling R, Bateman RJ, Morris JC, Laske C . Relationship between physical activity, cognition, and Alzheimer pathology in autosomal dominant Alzheimer's disease. Alzheimer's & Dementia: The Journal of the Alzheimer's Association, Sept. 25, 2018, In Press
Annotate
To make an annotation you must Login or Register.

Comments
University of Bologna
The paper by Mueller et al. demonstrates for the first time the existence of an association between self-reported physical activity and cognitive status even in patients with Alzheimer’s disease of genetic origin. The paper is interesting and well-conducted, with multiple measures of outcome (cognitive performance, functional status and CSF biomarkers).
The main limitation of the study, as acknowledged by the authors, is its cross-sectional nature, which only allows the demonstration of associations, but not of cause-effect relationships. After reading this paper, one would still like to know whether a high level of physical activity does improve cognitive status or, vice versa, whether the patients with cognitive deficit are prone to perform less physical activity.
Still, this paper favors the idea that physical activity may be considered an important therapeutic tool in patients at risk of cognitive decline, including those with autosomal dominant AD.
The paper is interesting and is consistent with a lot of other research that seems to indicate a protective association between exercise and the risk of AD, dementia, and cognitive performance.
It's a bit different in that the population involves people with a risk of a rare form of genetic AD that predominantly effects younger people. It's also cross-sectional—and add to that what seems like those people in the mutation carrier group for some reason had higher levels of exercise. Overall, to have 70 percent of any group reporting 150 minutes of physical activity per week indicates to me this is not a typical population.
But the authors’ point that they are the "first to support a beneficial effect of PA ... in genetically driven autosomal-dominant AD" is interesting. The more interesting results will be when they can report longitudinal data and have endpoints that are not based on estimated year to onset (EYO).
Banner Alzheimer's Institute
The article by Müller and colleagues provides compelling cross-sectional data on the relationship between physical activity, cognition, functional ability, and Alzheimer’s disease biomarkers in an autosomal-dominant AD population. As the authors stated, it will be important to examine this longitudinally. Although we are not collecting information on physical activity in the Alzheimer’s Prevention Initiative (API) Autosomal-Dominant AD trial, we have the possibility of doing so in the API Colombia Registry and API BIO cohorts. Our colleagues at the University of Antioquia and Massachusetts General Hospital are collecting information on physical activity as part of the observational biomarker study with the Colombian kindred and with plans to examine the impact of physical activity on cognitive decline and brain dysfunction, including on AD biomarker measures.
Boston University Chobanian & Avedisian School of Medicine
Since most people do not get sufficient exercise, it would be interesting to determine if exercise-induced changes in expression levels of antioxidant enzymes such as glutathione-S transferase play a role in the protection observed in this study. Such studies could be performed relatively quickly in rodent models.
Make a Comment
To make a comment you must login or register.