In TRAILBLAZER, Plasma GFAP Falls, but NfL Continues to Rise
Quick Links
A top contender among amyloid immunotherapies, donanemab lowered plaque load in the Phase 2 TRAILBLAZER trial. As reported last year at AAIC, this swift amyloid removal was accompanied by a drop in plasma p-tau217. Now, scientists led by Michael Pontecorvo of Avid Radiopharmaceuticals, a subsidiary of Eli Lily, report that plasma concentrations of glial acidic fibrillary protein (GFAP) also dropped over 18 months. In contrast, plasma neurofilament light (NfL), a marker of neurodegeneration, continued to climb in both treatment and placebo groups. The findings cast both p-tau217 and GFAP as sensitive biomarkers of amyloid plaques, and of their removal, but questioned if donanemab tempers neurodegeneration. The exploratory analysis was published October 17 in JAMA.
- In Phase 2, donanemab reduced plasma GFAP over 18 months.
- NfL continued to rise in both treatment and placebo groups.
- Plasma Aβ42/40 inched up similarly in both groups.
“Early, robust decline in plasma p-tau217 as a result of amyloid-reducing immunotherapy suggests that longitudinal assessment of this biomarker is valuable as a trial outcome measure, perhaps predicting clinical benefit and facilitating early phase dose selection,” commented Paul Aisen of University of Southern California in San Diego. “Along with the treatment effect on GFAP, it suggests downstream effects of amyloid removal on AD neurobiology.”
In a joint comment to Alzforum, Charlotte Teunissen and Lisa Vermunt of University Medical Center Amsterdam, noted that while previous studies have tied both p-tau217 and GFAP to amyloidosis, this does not necessarily mean those markers would work for monitoring amyloid removal in response to treatment. “But here, both markers pass the proof-of-concept for treatment monitoring response,” they wrote.
TRAILBLAZER enrolled 272 participants with early symptomatic AD whose PET scans showed that they had both amyloid and an intermediate level of neurofibrillary tangles in their brains. Volunteers randomized to the treatment group received monthly infusions of donanemab, which were halved when a person’s amyloid burden dropped below 25 centiloids. Volunteers were switched to placebo after amyloid dropped even further. By 24 weeks, donanemab had completely cleared plaques in 40 percent of participants in the treatment group, and by the end of the 76-week trial, nearly 70 percent had reached normal levels. The drug slowed decline on the Integrated Alzheimer’s Disease Rating Scale (iADRS) by 32 percent.
A highlight of last year’s AAIC meeting, Eli Lily scientists reported that p-tau217 dropped in step with the plummeting of amyloid plaques, falling by 24 percent in the treatment group compared to a 6 percent climb in the placebo group (Aug 2021 conference news).
The newly published work cements the exquisite sensitivity of plasma p-tau217 as a responsive biomarker. It also bolsters support that GFAP, a marker of glial activation, responds similarly. Pontecorvo and colleagues observed a significant dip in GFAP levels in the treatment group after 12 weeks. The gap between treatment and placebo groups widened thereafter, such that by the end of the trial, plasma GFAP levels had dropped by 12 percent in the treatment group but climbed by 15 percent in controls.
Furthermore, p-tau217 and GFAP dropped to a similar degree in people who were switched to placebo at 24 weeks due to complete amyloid clearance, and in those who continued treatment beyond 24 weeks. The data indicated that the markers fall in response to removal of plaques.
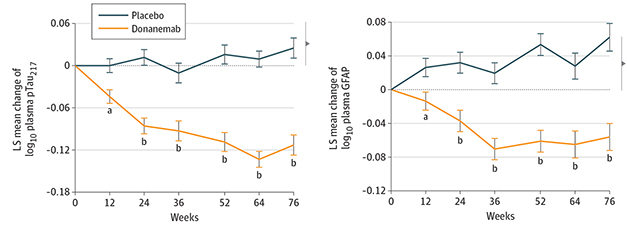
Plummeting with Plaques. Both p-tau217 (top) and GFAP (bottom) dropped significantly in people treated with donanemab over the 76-week TRAILBLAZER trial. [Courtesy of Portecorvo et al., JAMA Neurology, 2022.]
Over the 76 weeks, the dip in both p-tau217 and GFAP correlated with the drop in amyloid plaques, as gauged by amyloid-PET. The change in p-tau217, but not in GFAP, correlated with a reduction in tau tangles as measured by tau-PET.
While two other biomarkers the scientists measured changed over the course of the trial, they did not seem to be influenced by donanemab. Between baseline and 76 weeks, the plasma Aβ42/40 ratio crept up by 2 percent in the placebo group and by 4 percent in the treatment group. The difference between groups was only significant at 36 weeks.
NfL rose in both groups throughout the trial as well. At 76 weeks, it was 19 and 15 percent higher in the placebo and donanemab groups, respectively, than it was at baseline. The difference between the two groups was not significant.

NfL Keeps Climbing. Regardless of treatment group, plasma NfL continued to rise throughout the 76-week trial. [Courtesy of Pontecorvo et al., 2022.]
How would these four biomarkers track with brain atrophy and cognitive decline? The researchers found that only one—plasma NfL—correlated with brain atrophy, such that increasing NfL correlated with shrinking brain volume. Similarly, NfL was the only plasma biomarker measured that also tracked with the trial’s primary endpoint, change on the iADRS. In this case, NfL levels were slightly higher among people whose decline slowed the least.
Overall, the findings cast p-tau217 and GFAP as sensitive markers of amyloid and its reduction. The drop in p-tau217 also tracked with reduction in tau tangle burden, albeit not as significantly as it did with amyloid. This finding supports the idea that tau entanglement lies downstream of p-tau217, and that it may take longer for tau-PET signals to change in response to amyloid removal than for p-tau217 levels to fall, the authors suggested.
Why didn’t plasma NfL drop in response to donanemab treatment? For one, the authors noted that a slew of factors other than amyloid—from age to myocardial infarction to hypertension—are known to stoke plasma NfL. Secondly, they contend that there could be a time lag between the removal of Aβ pathology and its effect on NfL, which may not emerge within the 76-week trial.
Aisen agreed. “NfL, which is a relatively nonspecific marker of neurodegeneration, may reflect aspects of brain disease that do not change or take longer to change with amyloid-reducing therapy,” he said.
Mathias Jucker of the German Center for Neurodegenerative Diseases in Tübingen wrote that the NfL findings line up with recent work from his lab, wherein the researchers treated APP/PS1 mice with BACE inhibitors at different stages of amyloidosis. “We find a temporal uncoupling of amyloid and NfL changes in the CSF,” Jucker wrote (see Aug 2022 conference news). “When amyloid is reduced at stages when the brain is full of amyloid, CSF NfL still increases despite reduction of amyloid, which appears consistent with the results in this study.”
Teunissen and Vermunt raised yet another possibility, noting that NfL does not rise as much in AD as it does in other neurodegenerative diseases, including multiple sclerosis and spinal muscular atrophy, where the marker skyrockets. This modest increase in AD might provide less room for reduction, they wrote.
As to why Aβ ratios did not change in response to treatment, Aisen noted that immunoassays of Aβ ratios, which were used in the study, are not as accurate as mass spec assays, and may be influenced directly by immunotherapy, confounding interpretation. “Again, the huge amount of data expected soon will be very helpful to our understanding,” he wrote.
David Morgan of the Michigan State University in Grand Rapids noted that because the trial lacked cognitively normal volunteers, all of the participants likely already had elevated levels of neuroinflammatory and neurodegenerative biomarkers to begin with, indicating that even a modest reduction of these markers, such as the 12 percent dip in GFAP, is meaningful. Still, the biomarker findings jibe with the notion that there is a limit to how much amyloid removal can do to counteract cognitive decline, Morgan added. “Although longer treatment exposure may cause even greater reductions in neurodegeneration markers, there are factors other than amyloid which contribute to brain aging which most likely need to be addressed separately,” he wrote. “As for most therapies, anti-amyloid immunotherapy might be more effective as prevention instead of treatment.”—Jessica Shugart
References
News Citations
Further Reading
No Available Further Reading
Primary Papers
- Pontecorvo MJ, Lu M, Burnham SC, Schade AE, Dage JL, Shcherbinin S, Collins EC, Sims JR, Mintun MA. Association of Donanemab Treatment With Exploratory Plasma Biomarkers in Early Symptomatic Alzheimer Disease: A Secondary Analysis of the TRAILBLAZER-ALZ Randomized Clinical Trial. JAMA Neurol. 2022 Dec 1;79(12):1250-1259. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
USC Alzheimer’s Therapeutic Research Institute
Plasma p-tau217 measured by immunoassay or mass spectrometry has emerged as a tremendously valuable biomarker for AD pathology. Alone, or in combination with Aβ42/20 ratio by mass spec, plasma p-tau217 is an accurate predictor of amyloid PET and tau PET results, facilitating recruitment into early stage AD trials. Early, robust decline in plasma p-tau217 as a result of amyloid-reducing immunotherapy suggests that longitudinal assessment of this biomarker is also valuable as a trial outcome measure, perhaps predicting clinical benefit and facilitating early phase dose selection. Along with the treatment effect on GFAP, it suggests downstream effects of amyloid removal on AD neurobiology.
Results expected soon from the Phase 3 trials of lecanemab, gantenerumab, and donanemab will further clarify these issues. Why no effect on NfL and Aβ ratios? NfL, which is a relatively nonspecific marker of neurodegeneration, may reflect aspects of brain disease that do not change, or take longer to change, with amyloid-reducing therapy. Immunoassays of Aβ ratios are not as accurate as mass spec and may be influenced directly by immunotherapy, confounding interpretation. Again, the huge amount of data expected soon will be very helpful to our understanding.
VU University Medical Center
Amsterdam UMC, VU University
This paper examined the course of plasma biomarker changes in an exploratory analysis of the TRAILBLAZER Phase 2 trial targeting pyroglutamate amyloid isoforms using the donanemab antibody. The striking findings are the early, significant decreases of both plasma p-tau217 and GFAP levels, already at 12 weeks after treatment began. This suggests quite direct effects of amyloid lowering on two major players in the amyloid cascade, namely tau pathology and astrocyte activation. The changes in GFAP fit into prior findings of an association of this plasma biomarker with amyloid, such as the previously reported increased GFAP levels in amyloid-positive individuals. Nevertheless, even longitudinal increase of a biomarker along the disease trajectory is not proof of good potential for treatment monitoring. But here, both markers pass the proof-of-concept for treatment monitoring response.
Another striking finding is the lack of an effect on NfL. NfL is being used to monitor treatment responses in several neurological diseases, such as multiple sclerosis (MS) and several pediatric diseases, such as spinal muscular atrophy (SMA). What could be the reason for such a lack of effect in AD? It may be due to the less-pronounced increase observed for NfL in AD compared to, e.g., relapsing-remitting MS and SMA, providing less room for reduction. Another reason could be that NfL may rather reflect atrophy and white-matter alterations in AD, and the protective effects of amyloid lowering on these features have more long-term and more subtle temporal dynamics. This contrasts the rapid effects of anti-inflammatory treatments in MS, which lower NfL elevations caused by acute inflammatory-mediated axonal damage.
The next step is to prove that plasma p-tau217 and GFAP changes act as surrogates for cognitive change. These relations were weak in the current study, but, given cognitive outcome measures are usually variable, we need to await outcomes of Phase 3 trials to get a better sense of these relationships. On the other hand, the road to acceptance of these two plasma biomarkers as treatment monitoring markers is well paved by their correlation with amyloid reduction in the present study.
Michigan State University
These results complete the amyloid, tau, and neurodegeneration triad of biomarkers for TRAILBLAZER, demonstrating the utility of anti-amyloid immunotherapy. Although the percent reductions might seem small (12 percent for GFAP), the lack of a cognitively unimpaired group in the trial makes it hard to know what the baseline level of GFAP would be. In other work, cognitively unimpaired, amyloid-negative, older adults appear to have 50 percent less plasma GFAP than AD do cases, so the reduction is possibly 25 percent of the way back to "normal” (Benedet et al., 2021). This would appear to be in line with the roughly 30 percent slowing of cognitive decline with the anti-amyloid antibodies. This might be all that is expected given the observations that postmortem amyloid accounts for about a third of the variance in the rate of premorbid cognitive decline (Yu et al., 2021).
Although longer treatment exposure may cause even greater reductions in neurodegeneration markers, there are factors other than amyloid which contribute to brain aging that most likely need to be addressed separately. As for most therapies, anti-amyloid immunotherapy might be more effective as prevention instead of treatment.
References:
Benedet AL, Milà-Alomà M, Vrillon A, Ashton NJ, Pascoal TA, Lussier F, Karikari TK, Hourregue C, Cognat E, Dumurgier J, Stevenson J, Rahmouni N, Pallen V, Poltronetti NM, Salvadó G, Shekari M, Operto G, Gispert JD, Minguillon C, Fauria K, Kollmorgen G, Suridjan I, Zimmer ER, Zetterberg H, Molinuevo JL, Paquet C, Rosa-Neto P, Blennow K, Suárez-Calvet M, Translational Biomarkers in Aging and Dementia (TRIAD) study, Alzheimer’s and Families (ALFA) study, and BioCogBank Paris Lariboisière cohort. Differences Between Plasma and Cerebrospinal Fluid Glial Fibrillary Acidic Protein Levels Across the Alzheimer Disease Continuum. JAMA Neurol. 2021 Dec 1;78(12):1471-1483. PubMed.
Yu L, Boyle PA, Wingo AP, Yang J, Wang T, Buchman AS, Wingo TS, Seyfried NT, Levey AI, De Jager PL, Schneider JA, Bennett DA. Neuropathologic Correlates of Human Cortical Proteins in Alzheimer Disease and Related Dementias. Neurology. 2022 Mar 8;98(10):e1031-e1039. Epub 2021 Dec 22 PubMed.
BarcelonaBeta Brain Research Center; Hospital del Mar - Barcelona
The development of blood biomarkers for Alzheimer’s disease has been one of the most important advances in our field in recent years. We can now affirm that we have several blood biomarkers that accurately detect Alzheimer’s disease. In other words, blood biomarkers appear to be useful as diagnostic biomarkers or, in preclinical stages, as state biomarkers that indicate amyloid and tau pathology. This opens the door for using blood biomarkers for participant selection in clinical trials. Yet, blood biomarkers may also play other roles in drug development. Could blood biomarkers be used as pharmacodynamic/response biomarkers in clinical trials? The results of this study suggest so.
In this post hoc analysis of the TRAILBLAZER-ALZ Phase 2 randomized clinical trial, Pontecorvo et al. investigate the association of the anti-amyloid drug donanemab with the plasma biomarkers Aβ42/40, GFAP, NfL, and p-tau217 in early symptomatic Alzheimer’s disease. Plasma p-tau217 and GFAP were significantly lower in the donanemab treatment arm compared to the placebo one as early as 12 weeks after the start of the treatment, and their changes were associated with amyloid burden reduction as measured by positron emission tomography (PET). Of note, plasma p-tau217 and GFAP were still lower throughout the 76 weeks of the study even in those patients in whom treatment with donanemab was stopped at week 24 because amyloid PET levels dropped below 11 centiloids (CL).
These results indicate that plasma p-tau217 and GFAP could be used as target engagement biomarkers in clinical trials, that is, assessing whether the investigated drug has an effect on the target pathology (herein, Aβ pathology). In the future, these plasma biomarkers might also be helpful to select the dose to use in an eventual Phase 3 trial. These data are also in line with the notion that plasma p-tau217 and GFAP probably reflect Aβ dyshomeostasis and, albeit counterintuitive, it arises the question of whether these biomarkers should be part of the “A” (Aβ pathology) of the widely used ATN classification.
No significant changes were observed in plasma Aβ42/40 or NfL between the two study arms, except for an enigmatical increase in plasma Aβ42/40 in the treatment arm only at week 36. Plasma Aβ42/40 was measured with the Simoa Kit from Quanterix. One might ask whether using other Aβ42/40 assays (e.g., mass spectrometry-based assays) may lead to the same results. That plasma NfL does not correlate with amyloid or tau PET is not unexpected, since plasma NfL is a biomarker of neuronal injury that is not specific for AD. However, one would expect that if donanemab has an effect of halting neurodegeneration, plasma NfL would also decrease in the active treatment arm.
And here the big question arises: Could we also use blood biomarkers as surrogate endpoints in clinical trials? This study gives us a hint. A decline of plasma p-tau217 was associated with lower odds of exhibiting a meaningful worsening on the iADRS scale. The authors acknowledge the post hoc and explorative nature of this study. Larger and longer studies will be needed to test whether blood biomarkers are associated with slowing cognitive decline.
Make a Comment
To make a comment you must login or register.