Aiming at the Tangle’s Heart? DIAN-TU Trial to Torpedo Tau’s Core
Quick Links
Eisai’s anti-tau monoclonal antibody E2814 is the next investigational therapy to be evaluated in the DIAN-TU Next Generation secondary prevention trial. The Dominantly Inherited Alzheimer’s Network Trials Unit, an international trial platform in autosomal-dominant Alzheimer’s disease, announced on March 15 that its drug selection committee had chosen E2814 as the first anti-tau drug for its ongoing secondary prevention trial in carriers of pathogenic APP and presenilin 1 and 2 mutations. This DIAN-TU drug arm will start dosing in the fall.
E2814 is the first of what are to be three anti-tau arms in this adaptive platform trial (Bateman et al., 2017). The other two will be a small molecule and a genetic drug, but they have not been picked yet.
Eisai developed E2814 in its hunt for antibodies targeting the microtubule binding region. The MTBR has emerged as the next hot zone on tau, a protein of up to 441 amino acids, depending on how its six isoforms are spliced together. The MTBR starts at around amino acid 224 along tau’s sequence, downstream from its N-terminal and mid-domains. It is demarcated on one end by a caspase cleavage site at residue 224, and by residue 369 on the other end. In between lie the four repeat domains whose alternative splicing makes up the 3R or 4R forms of tau protein that are found in Alzheimer’s tangles and various other neurofibrillary deposits in related tauopathies.
The E2814 antibody recognizes an HVPGG sequence motif that occurs twice in tau’s MTBR, once in repeat 2 and again in repeat 4 (Roberts et al., 2020). This makes E2814 a bi-epitopic antibody—not to be confused with bi-specific, in which each arm of a synthetic antibody recognizes a different antigen.
MTBR aggregates form a core component of neurofibrillary tangles (Fitzpatrick et al., 2017). Moreover, scientists think the MTBR might be in the tau “seeds” that are thought to propagate through the brain. These seeds contain pieces of tau that include aggregation-prone hexapeptide motifs in the MTBR; they spread from one cell to the next and induce misfolding and aggregation of native, soluble tau in the recipient cell (e.g., von Bergen et al., 2000; Falcon et al., 2015).
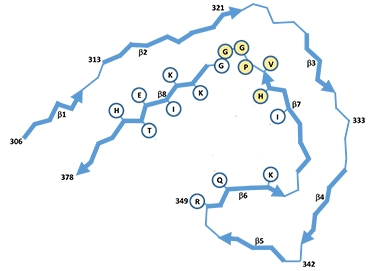
Right in the Middle. In this schematic of the C-shaped 3R/4R protofibril unit of Alzheimer’s tangles, yellow circles denote E2814’s second HVPGG binding motif in the R4 repeat. It also occurs in tau’s R2 domain (not shown). [Courtesy of Roberts et al., 2020.]
The first generation of investigational anti-tau antibodies in Alzheimer’s disease targeted tau's N-terminus, for example gosuranemab and semorinemab, or its C-terminus, such as RG7345. Alas, when they started posting underwhelming results in early clinical trials, drug developers shifted their gaze and are now zeroing in on the MTBR. E2814 binds a little ways downstream from UBC’s bepranemab, which binds residues 235 to 246, and near JNJ-63733657.
Also at the beginning of tau’s MTBR lies the 243-254 segment in tau’s R1 region that Kanta Horie, a scientist at Eisai, isolated and quantified in Alzheimer’s disease CSF last year, while working in Randy Bateman’s lab at Washington University, St. Louis (Dec 2020 news). The CSF concentration of this tau snippet rises as disease progresses, and it tracks closely with tau PET, hence it might make an informative biomarker in this upcoming DIAN-TU trial arm. WashU is the founding and central coordinating site of DIAN-TU.
E2814 is a humanized IgG1, i.e., it retains its effector function and may activate microglia to take up the antibody-tau complex for degradation. It has passed one Phase 1 safety trial thus far.
The DIAN-TU E2814 trial arm is supported by the NIA, philanthropic funders, and Eisai. During the first two years, it will measure the antibody’s effect on a range of biomarkers. If those results show target engagement, the trial will continue into a second two-year phase funded largely by Eisai, for which cognitive and clinical measures will be the primary outcome, Bateman told Alzforum.
This fourth DIAN-TU drug arm follows three prior arms that had targeted Aβ. Starting in 2012, DIAN-TU had tested solanezumab, which had negative results, gantenerumab, which missed the primary outcome but posted biomarker results strong enough to warrant an open-label extension, and the BACE inhibitor atabecestat, which stopped early due to that drug’s toxicity (Apr 2020 news).
The first two DIAN-TU trial arms have shown that presymptomatic and symptomatic mutation carriers differ too greatly in terms of their disease progression and performance on cognitive and clinical outcome measures to be combined into a single group (Apr 2020 conference news). “We learned that lesson,” Bateman said.
Therefore, the E2814 trial will group asymptomatic and symptomatic participants into separate, individually powered cohorts. Who is eligible? Mutation carriers ranging from 10 years younger than their family’s expected age at onset to 10 years after their symptoms began. This amounts to a 20-year span of Alzheimer’s disease progression. Asymptomatic participants will have negative tau PET scans at baseline, and their two-year primary outcome consists of fluid p-tau markers. Symptomatic participants will have positive tau PET scans at baseline, and their two-year primary outcome will be whether their tau PET reading went down. All participants will have neurodegeneration markers assessed. Along the way, they will donate blood and CSF, and take multiple brain-imaging scans and cognitive assessments such that a broad range of additional markers can be explored that the AD field is still learning about, Bateman said.
Longitudinal data in DIAN’s observational and earlier trial arms have shown that several phosphorylated forms of p-tau—181, 205, 217—rise in CSF and blood during the preclinical phase (e.g., Barthélemy et al., 2020). However, these fluid markers appear to rise no further once tau PET becomes positive around the time a carrier becomes symptomatic, or later as both symptoms and tau PET readings continue to increase. Intriguingly, the CSF concentration of MBTR-tau-243 does rise along with tau PET. To Bateman’s mind, this means that p-tau 181, 205, and 217 reflect the Aβ-driven tau pathophysiology that leads up the disease’s symptomatic phase, whereas CSF MBTR-tau-243 and tau PET reflect neurofibrillary tangles, i.e., deposited pathology. “These two types of markers are different in time, different in structure and, I believe, different in function, too,” Bateman said.
In a way, this trial is already happening, albeit without a drug. In early 2020, DIAN-TU began screening people for a so-called cognitive run-in period, in which participants undergo the trial’s tests, scans, and sample collection to establish both their individual baseline and their initial trajectory before taking an investigational drug to try to bend that trajectory back toward health. This design increases statistical power, a precious commodity in trials so small (Wang et al., 2019).
The pandemic has slowed recruitment into this prequel, but 60 people are “in” as of now, Bateman said. By the time the antibody is ready to be infused this fall, he hopes a majority of the anticipated 200 participants will be ready for randomization into drug or placebo. The trial is taking place at 35 sites in 13 countries.—Gabrielle Strobel
References
Therapeutics Citations
News Citations
- Tau Filaments from the Alzheimer’s Brain Revealed at Atomic Resolution
- MTBR-243 Tau: A Fluid Biomarker for Tangles Themselves?
- In DIAN-TU, Gantenerumab Brings Down Tau. By a Lot. Open Extension Planned
- Confused About the DIAN-TU Trial Data? Experts Discuss
Paper Citations
- Bateman RJ, Benzinger TL, Berry S, Clifford DB, Duggan C, Fagan AM, Fanning K, Farlow MR, Hassenstab J, McDade EM, Mills S, Paumier K, Quintana M, Salloway SP, Santacruz A, Schneider LS, Wang G, Xiong C, DIAN-TU Pharma Consortium for the Dominantly Inherited Alzheimer Network. The DIAN-TU Next Generation Alzheimer's prevention trial: Adaptive design and disease progression model. Alzheimers Dement. 2017 Jan;13(1):8-19. Epub 2016 Aug 29 PubMed.
- Roberts M, Sevastou I, Imaizumi Y, Mistry K, Talma S, Dey M, Gartlon J, Ochiai H, Zhou Z, Akasofu S, Tokuhara N, Ogo M, Aoyama M, Aoyagi H, Strand K, Sajedi E, Agarwala KL, Spidel J, Albone E, Horie K, Staddon JM, de Silva R. Pre-clinical characterisation of E2814, a high-affinity antibody targeting the microtubule-binding repeat domain of tau for passive immunotherapy in Alzheimer's disease. Acta Neuropathol Commun. 2020 Feb 4;8(1):13. PubMed.
- von Bergen M, Friedhoff P, Biernat J, Heberle J, Mandelkow EM, Mandelkow E. Assembly of tau protein into Alzheimer paired helical filaments depends on a local sequence motif ((306)VQIVYK(311)) forming beta structure. Proc Natl Acad Sci U S A. 2000 May 9;97(10):5129-34. PubMed.
- Falcon B, Cavallini A, Angers R, Glover S, Murray TK, Barnham L, Jackson S, O'Neill MJ, Isaacs AM, Hutton ML, Szekeres PG, Goedert M, Bose S. Conformation determines the seeding potencies of native and recombinant Tau aggregates. J Biol Chem. 2015 Jan 9;290(2):1049-65. Epub 2014 Nov 18 PubMed.
- Barthélemy NR, Horie K, Sato C, Bateman RJ. Blood plasma phosphorylated-tau isoforms track CNS change in Alzheimer's disease. J Exp Med. 2020 Nov 2;217(11) PubMed.
- Wang G, Aschenbrenner AJ, Li Y, McDade E, Liu L, Benzinger TL, Bateman RJ, Morris JC, Hassenstab JJ, Xiong C. Two-period linear mixed effects models to analyze clinical trials with run-in data when the primary outcome is continuous: Applications to Alzheimer's disease. Alzheimers Dement (N Y). 2019;5:450-457. Epub 2019 Sep 5 PubMed.
Further Reading
No Available Further Reading
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.