Scientists Propose a New Definition for Tau-Only Pathology
Quick Links
Tau tangles in the brain are an inevitable consequence of aging, and now a consortium of neuropathologists have coined a name for the condition: primary age-related tauopathy, or PART. They define PART mainly by what is missing; brains contain little if any Aβ. The consortium, led by first author John Crary of the Columbia University Medical Center in New York and senior author Peter Nelson of the University of Kentucky in Lexington, offer up the new term in a consensus paper in the October 28 Acta Neuropathologica online. “We see this pathology every day, but we have never had a name for it,” said Nelson. By christening the condition PART, he and his co-authors hope to instigate a wave of research on tau-only pathology.
PARTial Tauopathy.
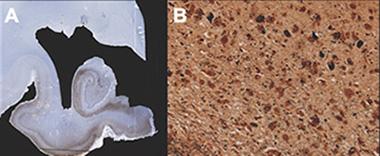
A section (left) from the medial temporal lobe of someone with PART exhibits extensive phospho-tau staining (brown). Right, silver stain picks up tau tangles (dark spots). [Image courtesy of Jean-Paul Vonsattel, Columbia University Medical Center, New York.]
PART is a pathological phenomenon, diagnosed only at autopsy, consisting of tau tangles that permeate the medial temporal lobe. The person might have appeared neurologically healthy, had mild cognitive impairment, or even had dementia. Previously, neuropathologists labeled PART with a variety of terms, such as “tangle-only dementia.” Those were inappropriate, the authors argue, because most people with PART do not experience dementia or senility. "For people with tauopathy only, we had no diagnosis to give them,” Nelson said. “All we could say is they did not have Alzheimer’s disease.”
Reaction to the new definition was mixed. “What they are now renaming PART is something that has been commonly accepted for decades,” said John Morris of the Washington University School of Medicine in St. Louis. Morris was not involved in the study. “However, if this construct, PART, brings more interest and inquiry to this abnormality, then I am all for it,” he said. Study co-author David Knopman of the Mayo Clinic in Rochester, Minnesota, admitted that the new term may be a matter of semantics. "But it is really important semantics," he said.
Some pathologists questioned the necessity of the term, saying it simply represents a stepping-stone to AD. “PART is a subset of full-blown Alzheimer’s disease,” said Charles Duyckaerts of the Hôpital de La Salpetriere in Paris. In a commentary accompanying the paper, Heiko Braak and Kelly Del Tredici of the University of Ulm in Germany argued that with time, so-called PART cases will pick up amyloid pathology and become simply AD.
Knopman disagreed. He told Alzforum that tauopathy could exist apart from Alzheimer’s. “When you mix them together, that is the toxic brew,” he said. “I do not believe that there is any evidence that medial temporal tauopathy induces amyloidosis.” Morris agreed that not all tauopathy would culminate in AD.
Morris was concerned that the precise borders of PART seem fuzzy. Indeed, scientists are still debating where to draw the lines between no pathology, PART, and AD, Nelson said. How much amyloid must be present to stop calling a case PART and label it Alzheimer’s? On the other end, even 20-somethings can show evidence of tauopathy in the brain (Elobeid et al., 2012), so when does that reach the level a pathologist should designate PART?
“PART, in some sense, is an inevitable consequence of aging,” Knopman said. Nelson said everyone who lives long enough will get PART, but the tauopathy appears to halt in the medial temporal lobe so long as Aβ does not get involved and spark Alzheimer’s. But even though it’s part and parcel of normal aging, that does not mean PART is harmless, Nelson said. He compared it to osteoarthritis, an unavoidable and uncomfortable consequence of aging. For some elderly individuals, osteoarthritis is no big deal. For others, it is crippling, so a cure would be a good thing, Nelson points out. Similarly, even if PART interfered with thinking in only some people, he said, it would still be worth identifying and fixing.
PART differs from some other tau-only conditions in that it typically contains both the 3- and 4-repeat forms of tau. Frontotemporal dementia usually has one or the other, Knopman noted. Progressive supranuclear palsy and corticobasal degeneration display mainly 4R tau, while Pick’s disease has mostly 3R.
Knopman said PART likely overlaps substantially with another condition defined by a lack of Aβ, called suspected non-AD pathophysiology, or SNAP. As with PART, people with SNAP may be cognitively normal or impaired. They show evidence of neurodegeneration in the form of hippocampal atrophy, altered uptake of glucose in the brain, or increased tau and phospho-tau in the cerebrospinal fluid, all without any sign of Aβ on PET scans (see Aug 2013 conference news story). However, while SNAP is diagnosed clinically in living people, PART can only be confirmed at autopsy, based on tau staining.
That could soon change. “As tau imaging is emerging, it is becoming clear that many cognitively normal people have evidence of at least low and sometimes moderate tau in their brains, much as the pathologists have observed,” commented Brad Dickerson of Massachusetts General Hospital in Boston, who was not involved in the study (see full comment below). Duyckaerts also predicted that within a few years, tau imaging combined with amyloid scans will allow researchers to determine once and for all whether the tauopathy Nelson and colleagues call PART always leads to amyloidosis and Alzheimer’s.
That is just one of many questions researchers have about PART, no matter what they choose to call it. Morris would like to know if PART underlies common complaints of aged individuals, such as difficulty remembering names. Nelson wondered why tauopathy typically pauses in the medial temporal lobe unless Aβ prods it onward. Crary and colleagues also asked what causes PART and how it fits with other neurodegenerative conditions, such as FTD. “[PART] patients have the potential to teach us a tremendous amount about the pathogenesis of neurodegenerative disease,” wrote Crary in an email to Alzforum.—Amber Dance
References
News Citations
Paper Citations
- Elobeid A, Soininen H, Alafuzoff I. Hyperphosphorylated tau in young and middle-aged subjects. Acta Neuropathol. 2012 Jan;123(1):97-104. PubMed.
Further Reading
Papers
- Ferrer I. Defining Alzheimer as a common age-related neurodegenerative process not inevitably leading to dementia. Prog Neurobiol. 2012 Apr;97(1):38-51. PubMed.
- Hawkes CA, Carare RO, Weller RO. Amyloid and tau in the brain in sporadic Alzheimer's disease: defining the chicken and the egg. Acta Neuropathol. 2014 Apr;127(4):617-8. Epub 2014 Jan 23 PubMed.
- Mandler M, Walker L, Santic R, Hanson P, Upadhaya AR, Colloby SJ, Morris CM, Thal DR, Thomas AJ, Schneeberger A, Attems J. Pyroglutamylated amyloid-β is associated with hyperphosphorylated tau and severity of Alzheimer's disease. Acta Neuropathol. 2014 Jul;128(1):67-79. Epub 2014 May 27 PubMed.
- Morris GP, Clark IA, Vissel B. Inconsistencies and controversies surrounding the amyloid hypothesis of Alzheimer's disease. Acta Neuropathol Commun. 2014 Sep 18;2:135. PubMed.
- Boluda S, Toledo JB, Irwin DJ, Raible KM, Byrne MD, Lee EB, Lee VM, Trojanowski JQ. A comparison of Aβ amyloid pathology staging systems and correlation with clinical diagnosis. Acta Neuropathol. 2014 Oct;128(4):543-50. Epub 2014 Jun 12 PubMed.
- Kua EH, Ho E, Tan HH, Tsoi C, Thng C, Mahendran R. The natural history of dementia. Psychogeriatrics. 2014 Sep;14(3):196-201. PubMed.
- Okamura N, Harada R, Furumoto S, Arai H, Yanai K, Kudo Y. Tau PET imaging in Alzheimer's disease. Curr Neurol Neurosci Rep. 2014 Nov;14(11):500. PubMed.
- Jack CR Jr. PART and SNAP. Acta Neuropathol. 2014 Nov 8; PubMed.
News
- Biomarkers Predict Alzheimer’s, But Shoe Does Not Always Fit
- Together, Aβ and Neurodegeneration Spell Cognitive Decline in Three Years
- Scan by Scan, Growing Tau PET Data Picks Up Early Memory Deficits
- Do Tau Tracers Track Cognitive Decline in Disease?
- Tau Tracers Shine at Boston Conference
- New Neuropathologic Guidelines for AD Almost Ready for Primetime
- Noisy Response Greets Revised Diagnostic Criteria for AD
Primary Papers
- Crary JF, Trojanowski JQ, Schneider JA, Abisambra JF, Abner EL, Alafuzoff I, Arnold SE, Attems J, Beach TG, Bigio EH, Cairns NJ, Dickson DW, Gearing M, Grinberg LT, Hof PR, Hyman BT, Jellinger K, Jicha GA, Kovacs GG, Knopman DS, Kofler J, Kukull WA, Mackenzie IR, Masliah E, McKee A, Montine TJ, Murray ME, Neltner JH, Santa-Maria I, Seeley WW, Serrano-Pozo A, Shelanski ML, Stein T, Takao M, Thal DR, Toledo JB, Troncoso JC, Vonsattel JP, White CL 3rd, Wisniewski T, Woltjer RL, Yamada M, Nelson PT. Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol. 2014 Dec;128(6):755-66. Epub 2014 Oct 28 PubMed.
- Braak H, Del Tredici K. Are cases with tau pathology occurring in the absence of Aβ deposits part of the AD-related pathological process?. Acta Neuropathol. 2014 Dec;128(6):767-72. Epub 2014 Oct 31 PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
Massachusetts General Hospital
It has been known for more than 20 years that many older people can have tau pathology in the brain without evidence of amyloid or other pathology. The older people are, the more common this is. It is not clear how tau-only pathology affects people, but it may be associated with memory loss. The authors of this paper should be commended for providing a new conceptual framework for pathologists to use when describing this feature in postmortem brain tissue. This will almost certainly open the door to much more study.
Until now, it has not been possible to study this entity before death. Things are changing. As tau imaging is emerging, it is becoming clear that many cognitively normal people have evidence of at least low and sometimes moderate tau in their brain, much as the pathologists have observed. We are now poised to begin to study how common this is, the implications of this observation with regard to people's cognitive function, and how it affects them over time. This new paper will provide an important foundation for linking the imaging observations with pathology, and for discussing this tau pathology as an entity in its own right, not necessarily as a part of a neurodegenerative disease with other pathology (such as amyloid).
View all comments by Brad DickersonMake a Comment
To make a comment you must login or register.