New Alzheimer’s and Parkinson’s Immunotherapy Data at AAN
Quick Links
For neurodegeneration researchers, highlights at the 2018 conference of the American Academy of Neurology, held April 21–27 in Los Angeles, California, were centiloid analysis of PET scans, the latest cognition update from people treated with the anti-Aβ antibody aducanumab, as well as new data from Parkinson’s patients on an anti-α-synuclein antibody. “The inclusion of results in centiloids is an important development,” Chris Rowe, University of Melbourne, Australia, wrote to Alzforum. “It will allow a more meaningful comparison of the cohorts’ baseline amyloid burden, and the effectiveness of amyloid clearance, [with those measures] in other drug trials, something that is otherwise limited by the use of different amyloid tracers and analysis methods. This is exactly why the centiloid method was developed.”
- Centiloid scale opens aducanumab PET data to comparison with other drug programs.
- In a very small cohort, aducanumab may be slowing three-year cognitive decline.
- At first blush, an anti-α-synuclein antibody appears safe in Parkinson’s patients.
Opening the first session on clinical trials in neurodegenerative diseases, Samantha Budd Haeberlein, Biogen, Cambridge, Massachusetts, presented 24- and 36-month data from the ongoing, long-term extension of the Phase 1b PRIME trial. PRIME tests the safety, tolerability, pharmacodynamics, and pharmacokinetics of aducanumab in people with prodromal and mild Alzheimer’s disease. As reported at CTAD last year, by 18 months amyloid deposition in people receiving the highest dose of aducanumab, 10 mg/kg, had dropped below the preset threshold for amyloid positivity—in this case a whole-brain standardized uptake value ratio (SUVR) of 1.1 for florbetapir PET (Dec 2017 conference news).
At ANN, Budd Haeberlein reported the PET data fitted to the Centiloid scale, which was designed to harmonize PET data across different tracers and detection systems (Klunk et al., 2015; Nov 2014 news; Feb 2013 news). “Different scanners, tracers, and even analysis methods contribute to the absolute numbers we see with SUVRs,” she said. “Essentially, the Centiloid scale is an attempt to standardize quantitative measures of PET imaging.” Other groups are adopting the scale, including ADNI-3 (Weiner et al., 2017; Jack et al., 2017; Yun et al., 2017).
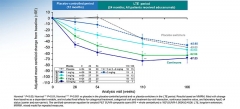
Say It in Centiloids. Brain amyloid deposition fell by 70 centiloids over 36 months in people with mild or prodromal AD who were treated with aducanumab. [Courtesy of Biogen.]
As expected, the shape of the Centiloid and SUVR graphs look the same, with florbetapir binding falling in an aducanumab dose- and time-dependent manner. “So what have they gained by the conversion to centiloids?” asked the scale’s creator, William Klunk, University of Pittsburgh. “Now the absolute value of the decrease holds some meaning that is generalizable to past or future studies,” he wrote to Alzforum.
In PRIME, amyloid continued to fall up to 110 weeks in people on the 6 mg/kg and 10 mg/kg doses, then leveled off by week 166 at a reduction of about 70 centiloids below baseline for both doses. People on 3 mg/kg tended to keep losing amyloid to week 166, as did those who started the trial taking 1 or 3 mg/kg or placebo, but switched to 3 or 6 mg/kg after the 12-month placebo-controlled period.
Rowe and Klunk were impressed with the 60-70 centiloid reduction. Klunk thinks the data imply a high level of target engagement. Whereas the key question had been whether anti-Aβ antibodies could meaningfully reduce amyloid deposition, now researchers can ask if amyloid is the right target, if treated early enough, he wrote.
Exploratory clinical data hint that, possibly, it might. Certainly that’s the big hope. Budd Haeberlein presented new data suggesting a continued benefit of aducanumab over time on the Mini-Mental State Exam (MMSE) and the clinical dementia rating sum of boxes (CDR-SB) scales (image below). The antibody slowed decline, suggesting it may have modified the disease process, but did not halt it. The effect was dose-dependent with the curious exception of the 6 mg/kg dose, which has been out of synch with the 3 mg/kg and 10 mg/kg doses since the early days of the trial. Budd Haeberlein did not explain this anomaly, but instead emphasized that the sample size is small, with only 166 people dosed in the first, placebo-controlled year of the study, and 117 continuing in the long-term extension. Other researchers have noted that the 6 mg/kg group began treatment at a different time than the 1, 3, and 10 mg/kg group.

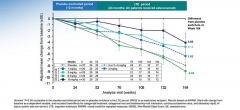
Did Cognitive Decline Slow? In general, people on aducanumab had better CDR-SB (top) and MMSE (bottom) scores than those on placebo. [Courtesy of Biogen.]
Gil Rabinovici, University of California in San Francisco, complimented the work. He asked about the relationship between the Aβ-PET reduction and the change in clinical outcomes. Did people with more amyloid removal do better? Budd Haeberlein responded that in 2016, Biogen observed that people who had a reduction of 0.15 SUVR units or more indeed were more likely to benefit clinically, but the company has not yet updated the analysis.
Summarizing the latest data on amyloid-related imaging abnormalities, Budd Haeberlein said ARIA usually occurred early in the course of treatment, was typically mild and asymptomatic, and tended to resolve or stabilize within four to five weeks. She concluded that, altogether, the PRIME data support further investigation of aducanumab in the ongoing Phase 3 EMERGE and ENGAGE trials.
On to Parkinson’s
In Los Angeles, Biogen also presented new clinical data on BIIB054, a monoclonal antibody that binds pathological, aggregated α-synuclein. Miroslaw Brys said that BIIB054 is approximately 400 times more selective for aggregated α-synuclein than for the monomeric form of the protein. At the AD/PD conference in Vienna, Biogen reported on the safety, tolerability, and pharmacokinetics of BIIB054 in healthy volunteers (May 2017 conference news). At AAN, Brys presented the first results of a cohort with Parkinson’s disease (PD) patients in the same Phase 1 clinical trial.
Thirteen men and five women with early PD, aged 47–75, received a single intravenous dose of either 0, 15, or 45 mg/kg of BIIB054. Nine were on no PD medication, five were on levodopa, two on rasagiline, and two on both rasagiline and levodopa. Over the next 16 weeks, participants underwent clinical assessments, two MRI scans, and had blood and cerebrospinal fluid (CSF) drawn to track BIIB054 levels and immune response to the antibody.
Brys reported that the pharmacokinetics of the antibody in patients were similar to those in healthy volunteers—it had a 33-day half-life in serum, reached a plasma concentration approximately threefold higher in the high- than in the low-dose group, while only 0.4 and 0.3 percent found its way into the CSF in the high- and low-dose groups, respectively. None of the patients developed anti-BIIB054 antibodies.
Brys said that as in healthy volunteers, BIIB054 formed complexes with α-synuclein in plasma. That both doses formed similar amounts of complex suggested near-complete saturation of blood synuclein with antibody. Attendees wondered why the antibody bound so much plasma synuclein if its affinity for monomers was so low. Brys explained that, although BIIB054 is more selective for aggregated than soluble α-synuclein, at high doses it is expected to bind the soluble form. Brys said there were no serious adverse events, and no obvious worsening of PD symptoms in either placebo or treatment arms during this short trial. The SPARK Phase 2 study of BIIB054 is enrolling now.—Marina Chicurel
References
Therapeutics Citations
News Citations
- 10th CTAD: Finally, Alzheimer’s Field Is Serious About Prevention Trials
- Paper Alert: Centiloid Scale Aims to Unify Amyloid PET
- HAI—Standardizing Amyloid PET: The Centiloid Project
- α-Synuclein Antibodies Enter Phase 2, Sans Biomarker
Paper Citations
- Klunk WE, Koeppe RA, Price JC, Benzinger TL, Devous MD Sr, Jagust WJ, Johnson KA, Mathis CA, Minhas D, Pontecorvo MJ, Rowe CC, Skovronsky DM, Mintun MA. The Centiloid Project: standardizing quantitative amyloid plaque estimation by PET. Alzheimers Dement. 2015 Jan;11(1):1-15.e1-4. Epub 2014 Oct 28 PubMed.
- Weiner MW, Veitch DP, Aisen PS, Beckett LA, Cairns NJ, Green RC, Harvey D, Jack CR Jr, Jagust W, Morris JC, Petersen RC, Salazar J, Saykin AJ, Shaw LM, Toga AW, Trojanowski JQ, Alzheimer's Disease Neuroimaging Initiative. The Alzheimer's Disease Neuroimaging Initiative 3: Continued innovation for clinical trial improvement. Alzheimers Dement. 2017 May;13(5):561-571. Epub 2016 Dec 5 PubMed.
- Jack CR Jr, Wiste HJ, Weigand SD, Therneau TM, Knopman DS, Lowe V, Vemuri P, Mielke MM, Roberts RO, Machulda MM, Senjem ML, Gunter JL, Rocca WA, Petersen RC. Age-specific and sex-specific prevalence of cerebral β-amyloidosis, tauopathy, and neurodegeneration in cognitively unimpaired individuals aged 50-95 years: a cross-sectional study. Lancet Neurol. 2017 Jun;16(6):435-444. Epub 2017 Apr 26 PubMed.
- Yun HJ, Moon SH, Kim HJ, Lockhart SN, Choe YS, Lee KH, Na DL, Lee JM, Seo SW. Centiloid method evaluation for amyloid PET of subcortical vascular dementia. Sci Rep. 2017 Nov 24;7(1):16322. PubMed.
External Citations
Further Reading
Papers
- Budd Haeberlein S, O'Gorman J, Chiao P, Bussière T, von Rosenstiel P, Tian Y, Zhu Y, von Hehn C, Gheuens S, Skordos L, Chen T, Sandrock A. Clinical Development of Aducanumab, an Anti-Aβ Human Monoclonal Antibody Being Investigated for the Treatment of Early Alzheimer's Disease. J Prev Alzheimers Dis. 2017;4(4):255-263. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.