Olfactory System Model Explores Antimicrobial Role for α-Synuclein
Quick Links
The delicate tissues that line our nasal passages form a barrier between the environment and our brain. However, current mouse brain dissection techniques usually toss aside this tissue, even though Heiko Braak, Ulm University, Germany, and other scientists consider it important in the pathogenesis of Parkinson’s disease (PD). To take a closer look at the nasal cavity, its vulnerability to infection, and α-synuclein expression there, scientists have developed a new technique that preserves the entire olfactory system of a mouse by keeping intact the head—nose, teeth, and eyes, the whole shebang. Researchers led by Michael Schlossmacher, Ottawa Hospital Research Institute, Canada, used this method to visualize high levels of Parkinson’s-associated proteins in olfactory neurons. They also traced an infection as it progressed throughout the olfactory system into the brain. They report that α-synuclein plays a protective role against harmful microbes. The current study stops short of linking nasal infection with changes in α-synuclein; however, the method opens the door to future studies on how microbes affect α-synuclein expression and metabolism. The results appeared online May 5 in the Journal of Neural Transmission.
“The strength of this technique is the ability to visualize connections of the brain that aren’t routinely studied in mouse models,” said first author Julianna Tomlinson.

Complete Picture. By placing slices of mouse head under the microscope, scientists can see extra-cranial structures such as the sinuses above the tongue (T) and their connections to the brain. [Tomlinson et al., 2017. J Neural Transm.]
A close-up of the ethmoid sinus and olfactory bulb. [Tomlinson et al., 2017. J Neural Transm.]

Nasal Cavity.
The olfactory bulb, along with the gut, has been proposed as an initiation site for PD pathology (see Jul 2011 news; Braak et al., 2003; Del Tredici and Braak, 2016). Aggregates are found there decades before symptoms emerge. Some think that misfolded α-synuclein itself, or infectious agents or toxins from the environment that alter α-synuclein, could propagate trans-synaptically to the brain. This hypothesis has been difficult to study in rodents because the intricate nasal structures are typically destroyed when a brain is dissected and prepared for microscopic analysis.

Pervasive Protein.
Cells of the olfactory epithelium (OE) express α-synuclein (brown) from their dendrites to their axons, which bundle into a cranial nerve that passes through the bony cribiform plate (CP) to the brain. [Tomlinson et al., 2017. J Neural Transm.]
To solve this problem, Tomlinson and colleagues developed a technique they call “holocranohistochemistry.” Instead of lifting the brain out of the skull, this method prepares the whole head—including the dura mater, upper portions of the cervical spinal cord, and venous and lymphatic structures. After anesthetizing and killing the mouse, and separating the head, the researchers soak it in formic acid to dissolve calcium from the bony structures. Once soft, they preserve it in wax and slice it for mounting on slides. Subsequent staining revealed the complex network of olfactory receptor neurons and their nerve bundles, and how they connect to the brain.
Importantly, staining with α-synuclein antibodies in newborn and aged mice revealed abundant expression in the olfactory system (see image above right). This was true both in wild-type mice and α-synuclein A53T mice that overexpress human α-synuclein with a mutation linked to early onset PD. In olfactory receptor neurons, the protein turned up throughout—from the cells’ dendrites stretching to the nasal airways, to their cell bodies that traverse the olfactory epithelium, and all the way down their axons, which bundle together to form cranial nerve I. Tomlinson also saw tau expressed in the same spots.

Infection Path.
A few days after a virus is inhaled from the nose to the ethmoid sinus (ES), researchers use anti-viral antibodies (brown) to monitor the virus in dendrites and cell bodies of olfactory receptor neurons, as well as their axon bundles (arrows). [Tomlinson et al., 2017. J Neural Transm.]
Further testing the model’s ability to visualize neurodegenerative disease pathology in olfactory nervous tissue, Tomlinson and colleagues prepared the TgCRND8 mouse model that overexpresses mutant human APP. Their olfactory system also harbored Aβ plaques. Together, the data suggest all three proteins are expressed in the olfactory system in commonly used mouse models and can be analyzed for their role in disease pathogenesis, Tomlinson told Alzforum.
The scientists then used holocranohistochemistry to trace an acute viral infection that started in the nose in newborn wild-type mice. Sacrificing mice at different time points up to 10 days after inoculation, the researchers documented the march of reovirus-T3D from olfactory receptor neurons to these cells’ nerve bundles (see image above left). At the same time, the activity of microglia, as measured by an antibody to the microglial marker Iba1, flared up in the olfactory bulb, and infiltrating macrophages fought off infection in the olfactory epithelium and cranial nerve I. In parallel, the infection traveled from the nose to the lungs, spreading systematically. The ultimate brain infection came from a mix of olfactory and systematic sources. Virus invaded various regions of the brain, including the thalamus, midbrain, and cortex (see images below).
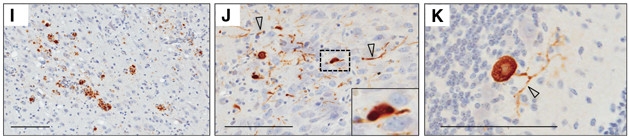
Brain infection: Anti-reovirus-T3D antibody finds the virus expressed in cells of the thalamus (I), midbrain (J), and cerebellum (K). [Tomlinson et al., 2017. J Neural Transm.]
What was α-synuclein up to in those infected neurons? One clue came from a paper by David Beckham, University of Colorado School of Medicine, Denver. He and colleagues reported that α-synuclein protected mice against West Nile virus in the brain (see Beatman et al., 2015). When infected, primary neurons pumped out more α-synuclein, which seemed to dampen viral replication. Mice lacking α-synuclein ended up with more virus in the brain and were less likely to survive.
To see if α-synuclein played a similar anti-microbial role in their model, Tomlinson infected newborn mice with reovirus-T3D, which causes a fatal brain infection in young pups. Indeed, α-synuclein knockouts succumbed more quickly than wild-type mice. Moreover, adult α-synuclein knockout mice injected in their tail veins with Salmonella typhimurium bacteria had a higher bacterial load in their spleens after five days. These data suggest α-synuclein has an antimicrobial function in innate immunity, wrote the authors. While they did not examine whether the infections directly affected α-synuclein in the olfactory system, Tomlinson said she next plans to examine the impact of chronic infection on α-synuclein metabolism in the nervous systems of older mice.
“I find this very intriguing,” said Patrik Brundin, Van Andel Research Institute, Grand Rapids, Michigan. “There seems to be a link between foreign microbes, be they virus or bacteria, and the triggering of synucleinopathy.” It should spur a lot of interest in understanding how foreign microbes trigger a boost in α-synuclein, he said, especially given mounting evidence that microbes in the gut influence α-synucleinopathies as well (see Sampson et al., 2016; Apr 2017 news). Brundin added that the holocranohistochemistry technique is potentially valuable, especially for researchers interested in studying the olfactory epithelium.
The survival effect in the current study was smaller than the one in Beckham’s, which he attributed to the different mouse models used. It will be important in future studies to probe the mechanism of α-synuclein’s antimicrobial abilities, Beckham told Alzforum. Interestingly, Aβ has also been proposed to function as an anti-microbial protein (see May 2016 news). “These proteins may have evolved in part to recognize harmful microbes and orchestrate an immune response that prevents infection of the nervous system,” Beckham told Alzforum.
If α-synuclein protein is protective against harmful microbes, and if pathogens make an environmental contribution to PD, then the data may suggest a new interpretation of the low CSF α-synuclein levels typically seen in PD patients, Tomlinson said. Perhaps reduced α-synuclein levels predispose a person to infection, and subsequent dysregulation kicks off the disease process. In essence, low CSF α-synuclein could represent a risk factor for Parkinson’s. Many believe it’s the other way around—that the lower protein levels result from the PD process already underway in nerve cells. Researchers conducting trials on therapies that seek to reduce α-synuclein long-term, and indeed Aβ, might be well advised to monitor for infection as a possible side effect, the authors recommended.—Gwyneth Dickey Zakaib
References
News Citations
- Parkinson’s: Thinking Outside the Brain’s Black Box
- Rumblings of Parkinson’s: Gut Microbiome Shifts in Early Stage of Disease
- Like a Tiny Spider-Man, Aβ May Fight Infection by Cocooning Microbes
Research Models Citations
Paper Citations
- Braak H, Del Tredici K, Rüb U, De Vos RA, Jansen Steur EN, Braak E. Staging of brain pathology related to sporadic Parkinson's disease. Neurobiol Aging. 2003 Mar-Apr;24(2):197-211. PubMed.
- Del Tredici K, Braak H. Review: Sporadic Parkinson's disease: development and distribution of α-synuclein pathology. Neuropathol Appl Neurobiol. 2016 Feb;42(1):33-50. PubMed.
- Beatman EL, Massey A, Shives KD, Burrack KS, Chamanian M, Morrison TE, Beckham JD. Alpha-Synuclein Expression Restricts RNA Viral Infections in the Brain. J Virol. 2015 Dec 30;90(6):2767-82. PubMed.
- Sampson TR, Debelius JW, Thron T, Janssen S, Shastri GG, Ilhan ZE, Challis C, Schretter CE, Rocha S, Gradinaru V, Chesselet MF, Keshavarzian A, Shannon KM, Krajmalnik-Brown R, Wittung-Stafshede P, Knight R, Mazmanian SK. Gut Microbiota Regulate Motor Deficits and Neuroinflammation in a Model of Parkinson's Disease. Cell. 2016 Dec 1;167(6):1469-1480.e12. PubMed.
Further Reading
Papers
- Park SC, Moon JC, Shin SY, Son H, Jung YJ, Kim NH, Kim YM, Jang MK, Lee JR. Functional characterization of alpha-synuclein protein with antimicrobial activity. Biochem Biophys Res Commun. 2016 Sep 16;478(2):924-8. Epub 2016 Aug 9 PubMed.
- Rey NL, Wesson DW, Brundin P. The olfactory bulb as the entry site for prion-like propagation in neurodegenerative diseases. Neurobiol Dis. 2016 Dec 20; PubMed.
Primary Papers
- Tomlinson JJ, Shutinoski B, Dong L, Meng F, Elleithy D, Lengacher NA, Nguyen AP, Cron GO, Jiang Q, Roberson ED, Nussbaum RL, Majbour NK, El-Agnaf OM, Bennett SA, Lagace DC, Woulfe JM, Sad S, Brown EG, Schlossmacher MG. Holocranohistochemistry enables the visualization of α-synuclein expression in the murine olfactory system and discovery of its systemic anti-microbial effects. J Neural Transm (Vienna). 2017 Jun;124(6):721-738. Epub 2017 May 5 PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.